Nihilism is best done by professionals. — Iggy Pop
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4924075/
https://www.apaservices.org/practice/ce/self-care/well-being
Nihilism is best done by professionals. — Iggy Pop
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4924075/
https://www.apaservices.org/practice/ce/self-care/well-being
Disclaimer: The following material was written for therapists to identify and manage patients with Borderline Personality Disorder (BPD), also known as Emotionally Unstable Personality Disorder, while illustrating some consequences that could occur during clinical practice. Clinical terminology will be interspersed with colloquial storytelling for accessibility. Attempting to conduct therapy with an undiagnosed or misdiagnosed mental health patient suffering from Borderline Personality Disorder can be like walking into the Australian Outback without a compass—clinical confusion, navigational errors, and emotional dehydration are virtually guaranteed. In essence, you won’t just be lost, you’re likely to become a part of the BPD landscape. The journey of a thousand mistakes begins with a stroll into the unknown. Furthermore, the following hypothetical situation in no way suggests that all patients suffering from BPD are similar regarding presentation, cognition, or behavioral responses. Therapists, like others, should avoid endorsing the No True Borderline fallacy. This essay is not intended as a support resource or treatment recommendation for those suffering from Borderline Personality Disorder; it represents an experiential and educational guide to inform and protect therapists from becoming professionally upended. Despite some of the behavioral depictions, occasional humor, and provocative vernacular, there is no motivation by the author to show prejudice or discriminate against this controversial and highly misunderstood mental health population. Contempt is reserved for the disorder (the legacy of trauma), but not for the person. However, without proper diagnosis and treatment, the person and their pathology are indelibly intertwined. Similarly, compassion is reserved for the person’s suffering, but not for their destructive behavior.
Having what is considered an externalizing disorder, people with BPD search for external sources of stimulation, validation, safety, and emotional regulation. Along their continuum of dependency needs, they also search for external sources of blame to avoid feelings of shame and accountability for whatever behavior is caused by their inability to self-regulate. The most frightening prospect for an untreated person with BPD, aside from abandonment, is being forced to confront their inner turmoil. Loved ones often describe relationships with Borderlines as “hostage situations,” but those who suffer from BPD are also held hostage by unresolved internal conflicts, insecurity, fear, impulses, and highly unstable emotions. For the most part, people with BPD are traumatized individuals who frequently seek corrective relationships that end up aggravating their condition while traumatizing significant others. Although human connection is considered vital for people with this condition to mitigate their fear of abandonment, interpersonal conflict is their habituated method for forming attachments because they conflate the vulnerability of closeness with abuse. They desperately need someone who really cares about their emotional pain and feelings of emptiness, but their lack of trust routinely results in destructive reactivity. In addition, their insatiable need to feel loved is saddled with a high degree of rejection sensitivity. As unfortunate as it is paradoxical, what a person with BPD desires the most is the very thing that perpetuates their pathos, and this no-win predicament often places caregivers in no-win situations. Subsequently, all things interpersonal are destined to become internecine unless intervention and long-term treatment are successful.
Borderline Personality Disorder is a serious mental illness that negatively affects the person suffering from it, in most cases, more than it affects those who interact with the disordered (approximately 10% percent of Borderlines commit suicide). Nonetheless, the consequences of this condition can be absolutely devastating for others due to its implacable and contentious nature. Overwhelmed by their emotions, patients with BPD can also overwhelm healthcare providers who try to treat them. Likewise, it’s common during crisis management for clinicians to feel responsible for the patient’s safety, needs, and the gravity of their despair. Borderline behavior is simply a maladaptive means of survival, but therapists must learn to recognize and manage the onslaught of such behaviors in a clinical setting. Therapists are professionally identified as caregivers, and many patients suffering from BPD obtain their sense of identity by being taken care of. Untreated Borderlines also believe that the love of a special person has the capacity to heal them, with the possibility of assigning this unrealistic responsibility to their therapist. This perilous juxtaposition creates the potential for a clinician’s version of Murphy’s Law and is made worse by the fact that Borderlines perceive boundaries as a form of neglect or rejection. Counterintuitively, conventional caregiving responses can exacerbate regression, which fuels dependency. Moreover, patients with BPD have problems with intimate relationships and people in positions of authority (a therapeutic relationship subsumes characteristics of both). Nonetheless, therapists should have compassion for those who suffer from this disorder, and for those who suffer by association. To be certain, untreated Borderline Personality Disorder creates a momentous ripple effect of consequences through personal, professional, family, and societal realms. We all pay a price in the end for the unaddressed legacy of this disorder. *The term Borderline (BPD) will be used for purposes of descriptive brevity, but this term is not meant to imply that a human being is reducible to their disorder (correctly identified as pwBPD).
Chaos is the score upon which reality is written. — Henry Miller
Although therapists may have the necessary academic background to assess Borderline Personality Disorder (BPD) from a vignette, list of traits, anecdote, or comprehensive case study, they may not have worked with enough varieties of Borderline experience in a clinical setting to identify the full range of behavioral manifestations. For example, therapists can learn to recognize common strains of the BPD “psychovirus,” but other strains may go completely unnoticed (i.e., not recognizing a melody because it’s being played backwards). The DSM-IV and DSM-5, with their checklists of infamous Borderline traits and diagnostic features, cannot begin to capture the experiential dynamics of being in a direct relationship with a Borderline individual (the World Health Organization’s ICD-10 defines BPD as Emotionally Unstable Personality Disorder). The complexity of this disorder sometimes goes undetected by even the most seasoned clinicians until specific traits or a behavioral pattern suggest a definitive pathology. In many ways, Borderline Personality Disorder is an abstraction that has to be interpersonally experienced to be believed. The danger of normalization, under diagnosis, misdiagnosis, and delayed diagnosis is common with Borderline patients because of the protean nature of this biosocial disorder and its wide array of individualized features. According to the article Subtypes of borderline personality disorder patients; a cluster-analytic approach from the journal Borderline Personality Disorder and Emotion Dysregulation, 2017: “The BPD population is notably heterogeneous from a descriptive and theoretical perspective. Two hundred fifty-six possible combinations of criteria may yield the same diagnosis. Hence, two patients with a diagnosis of BPD may have only one diagnostic criterion in common.” Correspondingly, a dimensional-based severity scale for BPD should include categories for mildly disturbed, moderately disturbed, and severely disturbed—in addition to Theodore Millon’s 4 BPD subtypes: Discouraged, Impulsive, Petulant, and Self-Destructive. Regarding functionality, some Borderlines are highly self-sufficient, whereas others can be completely dependent, yet they’re all emotionally dependent. BPD is considered to be the great masquerader of mental health disorders. As a characterological disorder, the symptoms of BPD are often camouflaged by the client’s mysterious presentation, myriad symptoms, and interpersonal conundrums, thereby making the prospects of a conclusive diagnosis even more troublesome. There’s also considerable overlap among all Cluster B disorders (narcissistic, borderline, histrionic, and antisocial). Approximately 90% of persons with BPD have co-occurring dependent, obsessive compulsive, or antisocial personality disorders. Unlike many other forms of psychiatric illness, BPD is neither self-limiting nor self-contained, although some symptoms may reduce with age. Overall, Borderline Personality Disorder should be considered on a broad psychiatric spectrum rather than relying on common caricatures, clinical stereotypes, or hyperbolized Hollywood depictions.
BPD represents approximately 2% of the general population with roughly 75% of cases being diagnosed among females, although the percentage of sufferers is likely equal among genders (women tend to seek treatment more often). A large percentage of people with BPD report a history of abuse in childhood (physical, emotional, and sexual), but yet 20% claim to have no memory of such encounters (possibly repressed or not recognizing emotional neglect as a form of abuse). In addition, we cannot underestimate the role of genetics as a primary factor in the development of the Borderline condition. As the late psychiatrist John Gunderson pointed out, “Our understanding of the disorder itself is in the process of dramatic change. Where its etiology was once thought to be exclusively environmental, we now know it is heavily genetic.” But even with all of these stipulations and appraisals taken into consideration, to creatively paraphrase Richard Feynman: If you think you understand Borderline Personality Disorder, you don’t understand Borderline Personality Disorder; just ask a Borderline. It’s Heisenberg’s uncertainty principle; it’s Schrodinger’s cat; it’s believing in two diametrically opposed ideas at the same time. As a system of trauma incognito, BPD passes the Turing test and takes therapists through a jungle of deception until they arrive in the uncanny valley. Considering the vast catalog of mental conditions, Borderline Personality Disorder stands out as an ontological contradiction that never fails to generate confusion among family members, loved ones, acquaintances, and caregivers. Most tragically, it deeply confuses the person who is suffering from it.
In terms of an accessible two-tier classification system, BPD “first impressions” could be described as either Authoritarian or Vulnerable, but assessments of personality disorders in general should incorporate a dimensional model that emphasizes quantitative measurement. *These non-clinical conceptualizations are only meant to depict distinctions in temperament and behavior as experienced by the non-borderline; they are supplemental rubrics designed to condense multiple subtypes.
Authoritarian BPD Interpersonal disposition: Compulsively self-sufficient, domineering, mesmerizing, intrusive, anxious, irritable, worrisome, dysphoric, demanding, passionate, presumptive, judgmental, perfectionistic, fearful, competitive, impatient, pessimistic, combative, easily angered, petulant, stubborn, critical, paranoid, and envious. Attachment style: Fearful/Preoccupied. Intimacy style: Erotophobic (fearing engulfment more than craving intimacy). Rationale: “I have needs for stability, predictability, and approval that were not met during childhood; therefore, I must be in charge to survive.” Valence: Aggressive, flamboyant, anxious, intense, and irritable. Parenting style: Over-involved. Level of functioning: Moderate to high. Objective: Control of self-image, others, and their environment (overtly expressed).
Vulnerable BPD Interpersonal disposition: Dependent, charming, captivating, coercive, desperate, mercurial, seductive, playful, hapless, passionate, anxious, perfectionistic, dysphoric, duplicitous, suspicious, solipsistic, fearful, affectionate, labile, docile, angry, hypersensitive, desultory, fantasy-prone, childlike, vindictive, self-destructive, and jealous. Attachment style: Disorganized. Intimacy style: Erotophilic (craving intimacy more than fearing engulfment). Rationale: “I have needs for safety, validation, love, and nurturing that were not met during childhood; therefore, I must be taken care of to survive.” Valence: Coy, mischievous, needy, desperate, and enigmatic. Parenting style: Under-involved. Level of functioning: Low to moderate. Objective: Control of self-image, others, and their environment (covertly expressed).
It should be understood that these classifications are not mutually exclusive; they represent qualitative conceptualizations with interchangeable overlap. For example, a Vulnerable BPD could easily switch into an authoritarian mode of expression, given the volatility of their internal barometer during stressful circumstances. However, general appearances indicate a default tendency towards either one disposition or the other, and both classifications maintain fantasies of omnipotence to offset deep feelings of insecurity. Ultimately, every character trait and behavior is on a continuum because BPD is a hybrid disorder that features significant similarities or comorbidity with mood disorders, behavioral disorders, and other personality disorders. Subclinical subtypes and colloquial descriptions, such as those incorporated in this essay, are convenient placeholders for purposes of conceptual taxonomy. Nonetheless, assessments of personality disorders in general should incorporate a dimensional model that emphasizes quantitative measurement.
For purposes of this essay, the author will focus on clinical encounters with the Vulnerable BPD patient on the severe end of the spectrum (i.e., impulsive or self-destructive subtype). It’s worth mentioning that it can be difficult for non-disordered individuals to think of some people with BPD as being “vulnerable” because of their propensity for aggressive, antagonistic, and antisocial behavior; but psychological fragility, regardless of its expression, is endemic to a fractured mind. Likewise, people with this disorder often display remarkable levels of resilience, defiance, and determination that suggests invulnerability. Their fear of abandonment might render them needy and childlike, but their fear of engulfment provides a surplus of resistance and pugnacious firepower. It can also be difficult for non-disordered individuals to comprehend arrested development in adults, emotional or otherwise, because of the sufferer’s ability to present themselves as if they were mature by blending in with other adults under favorable conditions. *Another archetypal rubric that is more qualitatively colorful is supplied by Christine Ann Lawson in her popular book Understanding the Borderline Mother.
In addition to the DSM’s notorious 9-point diagnostic criteria, here’s a 10-point list of the more “unspoken” aspects of Borderline Personality Disorder:
A useful image for Borderline Personality Disorder interpretation is to picture a 3-layer cake. On the surface of the cake is the person with BPD’s survival-based persona; a “false self” (coping self) that allows them to function in the world and feel accepted while avoiding the agony of criticism or rejection. In essence, the false self is an idealized form of identity that the Borderline wants to present to others as their authentic self. The middle section of the cake represents a large arsenal of primitive defense mechanisms, irrational thoughts, unstable emotions, and impulsive behaviors that generate the bulk of Borderline traits. The bottom layer of the cake symbolizes the traumatized and psychologically arrested inner child who is buried underneath a complicated mix of ingredients that include denial, fear, and dissociation. In therapy, clinicians must become the equivalent of psychoanalytical archaeologists willing to get messy in a mixing bowl of toxic cake batter to unearth the Borderline’s fragmented and empty core. Staying on the surface of the cake is what the BPD patient wants everyone to do, and they will fight like hell to maintain their protective exterior, but focusing on the frosting and its permutations only enables this evasive disorder to flourish with impunity. Basically, the “bright side” is the Borderline’s manifest image, and the “dark side” is their pathological behavior. Side A is a hit song, but side B should have never made it into the studio. As a result of such confusion, therapists and other providers often take an à la carte approach to symptom evaluation and treatment before getting to the center of the Borderline tootsie pop. But wait, there’s more! The therapist may assume that he or she is interacting with the patient’s “true self,” but this is an illusion. In reality, the therapist is interacting with a mask of normality (detached protector). However, the therapist will eventually be judged according to the Borderline’s impossible-to-please persona (angry-impulsive child). In fact, the patient’s sense of identity is deeply conflicted because they never developed trust, independence, healthy boundaries, or self-acceptance.
From an article entitled Two different presentations with Borderline Personality Disorder: “The earliest experiences for these patients were abusive. There were no good objects. Others either abused, tormented, and persecuted them or ignored, hated, and derided them. The child was helpless to have any effect on such a world; nothing they could do enlisted anyone to meet their needs for safety, security, and containment. From the viewpoint of the child, it was as if they truly must have been so bad that others, who should have cared for them, apparently had to punish them. It is important to understand that the patient cannot see the therapist as separate or as benign—as a therapist you are an Other to them. These patients often elicit a very warm, caring response. However, the sense of connection feels very fragile, because their core feeling is that they cannot affect the world around them and therefore that they do not exist to others. Their existence is invested in the Other, but the Other is not a real object for them, merely a repository for their projections.”
In recent clinical literature, Borderline Personality Disorder is considered a subtype of Dissociative Identity Disorder (formerly known as Multiple Personality Disorder) with various self-states (emotional states) in perpetual conflict with one another. BPD incorporates a polarized form of splitting (polarization of self, object, and relationship), whereas MPD/DID uses ego splitting or identity division. Borderline dissociation results in feeling completely different from moment to moment, but this also means that their feelings about others will alternate in an equally disorganized and unpredictable manner. People with BPD are the croupiers of emotional roulette, spinning their wheels of tribulation on an unstable table. In therapy, a Borderline patient will believe that their therapist is either an indifferent (cruel) professional or an unencumbered caregiver (loving parental representation) who has the power to rescue and nurture their wounded child persona. However, all therapists endorse a situational self by assuming the role of a caregiver as their occupational identity. In reality, the therapist is a human being with faults, problems, vulnerabilities, stressors, and limitations, just like everyone else. Last but not least, most interactions in therapy rely on neurotypical standards of reasoning and interrelating, but Borderlines have no reliable baseline for congruent communication or interrelatedness because of their fractured identity, cognitive deficits, emotional instability, abandonment anxiety, paranoia, dissociative amnesia, developmental immaturity, poor object relations, impulsivity, low distress tolerance, and lack of insight. To make matters worse, people with BPD are extremely sensitive to how others trigger their emotions, but they generally have no idea how they’re affecting the emotions of others. Introspection is replaced by deflection and projection. As a concluding cake topper, humans are social mammals, but Borderline Personality Disorder is a relational disorder with low personality organization and compromised social cognition. What could possibly go wrong?
“[People with] personality disorders exhibit chronic, pervasive problems getting along with people in all kinds of different contexts,” says Thomas R. Lynch, PhD, assistant professor of psychology at Duke University and the Duke University Medical Center. “And this includes therapists.”
It is certainly abnormal to crave so much to be loved and understood. — Anaïs Nin
A conceptual view of BPD is noted by Dr. Robert B. Shulman: “The characteristics of the borderline personality include a marked and persistent identity disturbance, chronic feelings of emptiness and boredom, and intense unstable personal relationships. The borderline tends to have difficulty tolerating being alone and will fear abandonment. They are highly impulsive, and may engage in self-mutilating behavior, have recurring suicidal threats, and manipulate others to meet their immediate needs. The borderline also tends toward having an intense affect; unstable mood; displays of inappropriate anger; perceptual distortions; and under great stress may depersonalize. They see the self as justified; since they feel intolerably bad, they are entitled to go by impulse instead of common sense and feel entitled to soothe themselves. Their fictitious goal is to do whatever they want as they cannot be happy by how others do it. Their methods are protean, and include splitting, primitive idealization, projective identification, denial, and devaluation. The borderline personality is not a cooperator. Their impairments include affective instability, anxiety and panic, and engaging in self-harmful behaviors. These impairments may cause significant interference in social or occupational functioning. Because the borderline uses others to meet their needs, they can often be the ‘problematic patient’ that medical offices dread.”
Borderline Personality Disorder could be thought of as a unique arrangement of C-PTSD (Complex Post-Traumatic Stress Disorder) that causes the sufferer to believe that some combination of love, validation, control, and retributive justice is the cure. However, this view is conceptually limited because it does not take into account heredity, object inconstancy, autophobia, feelings of emptiness, jealousy, and a sense of entitlement that creates an impaired character structure akin to a developmental syndrome with alloplastic and autoplastic defenses. Unlike other trauma-based disorders, the identity disturbance component of BPD means that they don’t know where they end and other people begin. In reality, BPD is an amalgamated adaptation to C-PTSD with novelty features that remain maladaptive. What emerges is a pathological split-self, otherwise known as structural dissociation—multiple self-states that represent a highly unstable entity of its own, like uranium or a dominant chord that never resolves. Because living in a dissociative state is incompatible with the exigencies of reality and healthy socialization, a protective narrative is constructed by the sufferer to make sense of the world. Furthermore, protective attachments (idealized others) are needed to compensate for regulatory deficits and the Borderline’s lack of identity congruence. In a dysregulated nutshell, Borderline Personality Disorder embodies emotional dependency beset by abandonment rage with an unhealthy serving of instability, insecurity, and immaturity. The Borderline’s attachment issues are pervasive and owe as much to insufficient bonding during infancy and childhood as they do to trauma-induced hypervigilance (the unstable sense of self originates from the internalization of the child’s primary relationships and the overall impact of developmental deficits). Perhaps most ironically, many individuals who become involved in a BPD relationship are later diagnosed with some form of PTSD themselves due to being recipients of the Borderline’s need for control and self-justified emotional reactivity (aka borderline abuse). Left to their own devices, Borderlines will not break the cycle of abuse, they will perpetuate it towards themselves and others.
Come on, babe on the round about; ride on the merry-go-round. — Robert Plant
The ways that Borderline Personality Disorder can present itself are sundry, but traits reliably surface whenever sufficient stressors are involved in the person’s life. The problem is that significant levels of stress may not emerge during casual therapy sessions as they would in a family context, romantic relationship, or adverse encounter. In many cases, the patient’s affable demeanor and energetic magnetism, as presented in a structured setting, can create the illusion of normalcy for extended periods of time before things begin to unravel. But to be sure, this commonly misunderstood disorder is a far cry from the “worried well” going through a seasonal spell. BPD is a form of psychological pain that cannot be attenuated by methods of normal communication, compassion, or reasoning. For the most part, individuals with personality disorders do not realize that their perceptions, emotions, and behaviors diverge considerably from quotidian human experiences. To be inappropriately blunt, Borderline “flare-ups” (episodes) behave a bit like the herpes virus. There may be no visible outbreak of symptoms until the person with BPD encounters enough stress and frustration to end the remission period that constituted the better angels of their nature. In most cases, the crux of this disorder is environmentally triggered by interpersonal factors and exacerbated because the host has a skewed perceptual lens. This is why those suffering from BPD can “hide” their internal suffering whenever social circumstances are at a minimum threat level. However, it’s the stress of not getting their way, especially with intimate others, that really brings out the creature features of this tumultuous disorder.
Borderlines want a normal and happy life, but they don’t know how to find that magical place; it’s like window shopping in the dark while wearing cataract shades. The lights are out on the mean streets, and there’s no hope to be found. They’re on the run for restitution, but they’re running in circles. A Borderline’s inability to manage stress or interact with others in a balanced way creates an amusement park ride of rotating pandemonium—it’s the repetitive pattern of a self-fulfilling cycle. For many people with BPD, life is just too difficult, or isn’t worth living. *It’s important to know that not all Borderlines engage in self-mutilation, suicidal ideation, or suicide attempts, but they can be self-destructive in other ways that are less obvious (i.e., negative internal dialogue, eating disorders, substance abuse, and other self-sabotaging behaviors). Furthermore, self-injury and suicidality for a person suffering from BPD are more about taking control of a shitty situation rather than “letting go.” In fact, studies have shown that Borderlines are less sensitive to physical pain than they are to emotional pain. Physical pain distracts from, alleviates, or brings attention to their psychological pain. Regarding other counterintuitive revelations, a BPD’s risky behavior (i.e., promiscuity, substance use, spending sprees) is usually enacted for purposes of escapism, self-soothing, displacement, or to feel alive, but it’s occasionally misinterpreted by others as recreational or transgressively adventurous. Since most humans have their vices when faced with adversity, a Borderline’s excuses for irresponsible, self-destructive, or hedonistic behaviors are sometimes viewed as contextually acceptable. As clinical misinterpretation progresses, the caregiver may end up pouring the equivalent of codependent jet fuel on the BPD patient’s emotional reasoning by gradually supporting their distorted views of reality and excuses for certain types of behavior, or by feeling compelled to gratify assorted requests for special favors due to their professed victimhood.
Borderlines could also be thought of as emotionally unstable individuals with maladaptive software programs—akin to a faulty GPS—when it comes to navigating interpersonal dynamics. Based on this analogy, Borderline Personality Disorder could be renamed Interpersonal Navigation Disorder with significant impairments when it comes to expressing needs, understanding self and others, and regulating emotions. According to the dictates of repetition compulsion, a person with BPD is playing musical chairs according to the exigencies of their dependency needs. In clinical terms, people with this disorder have a low personality organization (low emotional quotient); they experience exceptional difficulty when it comes to managing themselves (internal regulation) and interacting with others (poor social cognition). Because people with BPD were often betrayed by their original caregivers, they anticipate betrayal from anyone who is supposed to care. Unfortunately, the Borderline condition is not amenable to standard forms of patient engagement. In fact, some forms of therapy can actually make BPD patients worse by trying to accelerate self-sufficiency, because motivational interventions threaten their dependency needs. As a result, Borderline patients must be willing to submit to specialized treatment programs (i.e., DBT, MBT, TFP, and schema therapy) that can require years of attendance before adequate insight is developed and meaningful change occurs (some estimates suggest 2-8 years for remission and 8-16 years for recovery). *Effectively mitigating the deleterious effects of this disorder to improve the client’s quality of life is more realistic than expecting a “cure.” However, due to chronic instability, crisis intervention may be the only treatment some Borderline patients ever receive.
Longitudinal studies of patients with Borderline Personality Disorder indicate that even though these patients may gradually attain functional roles several years after admission to psychiatric facilities, still only about one-half will have stable, full-time employment or stable marriages. Nonetheless, overall treatment prognosis is good for dedicated patients with low comorbidity, and there are reported cases of spontaneous symptom remission with age (*remission is distinct from recovery). However, Zanarini et al. identified younger age as one of several predictors of earlier time to remission over 10 years of follow-up, challenging the belief that older age brings more improvement in BPD. It should also be noted that some people with BPD increase acting-out behaviors when they become older because their ability to ascertain attention declines, especially if validation was received for their physical appearance or social status during their prime. As a general rule, early diagnosis and treatment of BPD provides the best prognosis, but a reduction in specific symptoms, such as impulsivity, can occur with age. Regardless of major improvements in treatment approaches and clinical outcomes, many Borderline attitudes and behaviors persist indefinitely based on habituation. For others, their denial is too intransigent to accept diagnosis or commit to extensive treatment intervention. To even suggest that something might be wrong with a Borderline’s worldview is often considered a threat, and they will do whatever it takes to protect their fragile psychological territory. Hitting “rock bottom” for a person with this disorder generally means running out of people they can lean on until they’re forced to face themselves. Finding someone to subsidize their pathology is achieved through coerced caretaking, and this typically includes stories of victimization meant to justify learned helplessness. Architects of their own misery, seldom can they see or understand how lifelong patterns of emotionally unstable behavior (repetition compulsion) and infantile dependency needs continue to place them in unfortunate situations. Furthermore, because BPD dovetails with traits of Paranoid Personality Disorder, many patients with this disorder believe that those who are trying to help them are secretly trying to harm or take advantage of them. It could also be argued that this population would be better managed by clinicians who have additional training in child psychology due to the Borderline’s stunted psychological development and acting-out behaviors. As a general rule, people with BPD don’t know how to interact in relationships, and a relationship with their therapist is just another type of relationship.
“The clinician is challenged in many ways when caring for a patient with borderline personality disorder. The poor coping skills and tendency to form intense, unstable relationships associated with these patients often identifies them early on as difficult and problematic. Treatment compliance is poor, and their behavior is often demanding, although they reject help. They may often idealize the physician as the only person who offers help and understanding yet return for a follow-up visit expressing anger and hatred. The behavior of ‘splitting,’ or viewing one member of the healthcare team as all good while another is all bad, is common in these patients. It is important that all members of a medical staff or unit team have a consistent approach to avoid the manipulative behavior that splitting may cause,” states Dr. Melinda Lantz.
Things are not always what they seem. — Phaedrus
The challenge for clinicians is when an undiagnosed or misdiagnosed Borderline presents in multiple sessions without conspicuous traits or clear evidence of Cluster B psychopathology (misdiagnosis is a precursor for iatrogenic harm). Likewise, the patient’s clinical record is sometimes contradictory and misleading. The elusiveness of this disorder is fascinating because it often escapes the radar of clinicians due to the patient’s ability to superficially present themselves as well-mannered, amiable, energetic, and ostensibly reasonable during brief interactions. But this is not your average person who has found themselves in a bind. People with BPD can appear cognitively copacetic, well-adjusted, and highly functional (apparent competence) when engaged with specific activities that allow for structure, routine, affirmation, control, and unambiguous results. It should also be noted that Borderlines who are taciturn can be exceptionally difficult to assess because they often remain placid and “perfectly presentable” until provoked. Pretending that everything is fine is how people with this disorder hold themselves together in public, despite what occurs underneath their acting face. In other cases, pressured speech and excessive worry may indicate ongoing hyperarousal or a propensity for catastrophizing. If internal dysregulation (ego-dystonia), impulsivity, or mood lability is admitted by the patient, it’s notoriously misdiagnosed as Bipolar Disorder (the most common clinical misdiagnosis). Other candidates for misdiagnosis include atypical depression, ADHD, and an assortment of anxiety disorders. A tendency to minimize the patient’s problems frequently occurs because of the mismatch between how a person with BPD appears when they’re in a good mood versus how they behave when their composure wanes.
From the book Management of Countertransference with Borderline Patients: “Kernberg argued that the borderline concept is really a personality organization rather than a specific nosological entity. A variety of different personality disorders, including paranoid, antisocial, schizoid, infantile, narcissistic, and cyclothymic, all could be subsumed under the overarching ego organization.” Despite a plethora of comorbid considerations, a contradictory or confusing diagnostic history might well suggest that the client is suffering from pervasive patterns of psychological disturbance that transcend Axis I considerations. However, due to time constraints and other factors involved with high-volume clinical work, reliance on the assessments of previous caretakers often remains unquestioned. Likewise, it’s sometimes assumed that the patient has been an innocent bystander of chaotic family circumstances—surrounded by other personality disordered individuals—rather than being a card-carrying member themselves. In other words, objectivity can be lost if a confirmation bias exists in thinking that the patient is an unfortunate victim of bad luck instead of being a potential culprit (this bias does not dispute victimization from abuse in childhood). Whenever such misguided conclusions become diagnostically solidified, the lost-in-translation therapist becomes a detective chasing down the wrong suspects. The clinician might be in the right neighborhood, but they’re focusing on the wrong address. In these circumstances, understanding the multi-generational effects of trauma and the hereditary pervasiveness of Borderline Personality Disorder is of key importance (once again, early diagnosis of BPD is crucial for a favorable treatment prognosis).
Due to the public and professional stigma surrounding Borderline Personality Disorder, and because misdiagnosis is common, medication management is often chosen as the sine qua non for treating symptoms rather than subjecting the client to a series of more intensive evaluations, such as structured interviews. However, psychotropic medication is supplemental, at best, and not effective for addressing the nucleus of this multi-layered disorder. Unless it has been determined that the patient suffers from a comorbid mood disorder, a “skills not pills” approach to treatment is imperative. Unfortunately, most insurance companies do not cover payment for treatment of personality disorders due to the expected duration of multimodal intervention and indeterminacy of treatment outcomes. Revealing the disorder to the patient can also backfire because it suggests an inherent defectiveness, coupled with a long-standing societal stain. After all, how do you tell someone who is hypersensitive to criticism that they have a disorder that makes them hypersensitive to criticism? How do you tell someone who is resistant to change that there’s a lot that needs to be changed? How do you tell someone who lacks a sense of self that “they” have a disorder of the self? How do you tell someone who lives by emotions that their emotions are unreliable? How do you tell someone with cognitive deficits that they should exercise their cognition to overcome their deficits? How do you tell someone who lacks epistemic trust that they must trust an emotionally uncomfortable processes? How do you tell someone who fears abandonment that they must abandon everything they thought they knew about themselves and others? In essence, you’re insulting a Borderline’s essence. In addition, untreated people with this disorder are not entirely opposed to the idea of killing the messenger, especially when the messenger is delivering an unwelcomed message.
An overarching rubric for the evaluation of Borderline character pathology is supplied by psychologist Joseph W. Shannon:
It’s the Hard Knock Life for us. — Annie
Borderlines are known for being resource and sympathy acquisition specialists—chameleons of expediency and masters of mimicry with lifestyles that are frequently in dramatic fluctuation. Their lives are in flux because their moods and emotions are in flux. Their stories are captivating and their charismatic powers of persuasion are often unrivaled. The BPD’s voyage of hardship (unrelenting crisis) and methods of retelling are irresistible bait for any caretaker who cares too much. In fact, Borderlines are some of the most emotionally convincing interlocutors on the planet. From a BPD’s point of view, they’re soldiers of misfortune struggling for survival in a hostile world filled with untrustworthy people (survival usurps self-awareness). In many ways, Borderline Personality is a disorder that seeks vindication and compensation for suffering, hence the sense of entitlement. In addition to there being a discouraged subtype, it could be said that people with this disorder display profiles in discouragement. Because many people with BPD come from pathogenic families, they’ve learned to see other people as potential allies or enemies—eat or be eaten in the land of dysfunction. The Borderline’s street-fighter style of resilience is impressive, but it’s a maladaptive form of resilience based on hypervigilance, persecutory beliefs, and fraught with interpersonal jeopardy. Someone is either doing something to them or is not doing enough for them. Put-out and put-upon, but never in the wrong, people with BPD have an unusual knack for provoking circumstances whereby they can eventually declare themselves the victim. For people with this condition, validation of victimhood is one of their highest priorities. In fact, this self-fulfilling prophecy undergirds most of their disputatious interactions, sense of self, and subsequent rationalizations for destructive behavior. Assessments taken at face value may have therapists believing the client’s victim identity, which can provoke a strong rescue response, thereby enabling an unwarranted and unsustainable advocacy position as the therapeutic alliance develops. After all, it’s considered rude for therapists to question the veracity of a self-proclaimed victim in the safe space of a treatment setting. But keep in mind, the patient’s list of “abusers” often includes multiple offenders in multiple contexts to be blamed over an extended period of time. For example, Borderlines can go from one personal or professional relationship to another while complaining about how they were grievously mistreated during their last encounter (aka “support surfers,” “nomadic amnesiacs,” “emotional refugees,” and “professional victims”). Low-functioning Borderlines, for example, may exhibit significant patterns of social parasitism with recurring bouts of upheaval and displacement. Their last relationship or domestic situation is usually framed as being so traumatic that they deserve to be sheltered and supported ASAP. People with BPD will pull at your heartstrings, but there’s definitely some strings attached.
As an essential component to the victimhood sales pitch, the Borderline’s penchant for gossip is highly effective for collecting negative advocates (e.g., concerned others, enablers, and “flying monkeys”). Welcome to the triangulation trap—endorsing the innocence project with someone who may not be so innocent. When this happens, therapists may find themselves caught in the crossfire of a divide-and-conquer melodrama with an inclination to side with the patient. After all, therapists have a fiduciary responsibility to care for their clients. However, a detailed history of the patient’s former relationships will undoubtedly reveal significant contradictions while demonstrating evidence for repetition compulsion. Furthermore, these hard-luck stories are frequently incoherent and will shift over time. Borderlines are descriptively impressionistic about their own choices and conduct, but they’re emphatically convinced about the malevolence of their alleged persecutors. Skepticism and consultation are advised, because these self-pitying anecdotes are habitually inconsistent and often nonsensical when pressed for specifics. People with BPD are storytellers of omission; what they tell you may not be as important as what they leave out. In fact, the Borderline’s unconscious ability to identify as a victim in search of another abuser is so entrenched in their psyche that it easily qualifies as their most reliable self-fulfilling prophecy (Barnesian performativity)—propelled by the dark energy of automaticity—no matter how counterfactual or patently absurd.
Borderlines are notoriously involved with contentious divorces, custody battles, or complicated legal issues with former partners, family members, and professionals. BPD friendships are often perfunctory and run the gamut from parental confidants to “frenemies.” A Borderline’s opinions of other people can change quickly, and someone who is seen as a best friend one day may be considered a traitor the next. Because of their low threshold for betrayal, very few acquaintances are exempt from character assassination when a person with BPD declares emotional warfare. A Borderline’s history of interpersonal conflict is usually quite extensive before they step into a therapist’s office; however, these battles will often be framed as being unfair, cruel, and imposed upon them by malicious agents. If there’s a dispute, a person with BPD will declare themselves as virtuous while creating an exaggerated narrative regarding their “adversaries” (Borderlines seem to be unfamiliar with the mathematical concept of a common denominator). Most of their relationships are inherently adversarial because people with this disorder feel that other people are inherently untrustworthy. In most situations, Borderlines will unconsciously provoke confrontations to reassert victimization, thereby eliciting caretaking responses from others. *It’s difficult to think of someone as potentially dangerous when they’re claiming to be in danger, but dissimulation is a common form of misdirection with high-conflict people.
Having burned so many bridges, Borderlines are always looking for a new set of suspension cables. The BPD’s ongoing search for someone who “really cares” becomes a perpetual motion machine of dependency and disappointment. Upon closer examination, people with BPD inadvertently exploit others while maintaining a repeated position of victimhood—perpetuating a cycle of oppressor, victim, and rescuer. Consequently, this position abdicates personal responsibility while justifying the Borderline’s impulsive behavior, self-aggrandizement, rage, and mistrust of others. In other words, Borderlines are playing a game of emotional tennis without a net. Note to therapists: Never hand the ball to the worst player on the court. People with BPD are crucibles of disturbance who are exceedingly proficient at persuading their sympathizers that everyone else is disturbed; but in the Cluster B interrogation room, accusations are often confessions in disguise. Psychological projection, a BPD specialty, results in layers of confusion and misdirection that require labor-intensive analysis, discrepancy identification, and retrospective dismantling. For the most part, whatever a person with BPD doesn’t like about themselves or their behavior will be projected onto the nearest recipient.
To add to the farrago of misdirection, Borderline paranoia is profoundly bewildering and contagious if not understood for what it is. Paranoia is a projection of the Borderline’s aggression and perceptual distortions, but it also works to reinforce victimhood. Borderline Personality Disorder overlaps with Paranoid Personality Disorder, but it also includes affective and performative features that make the content of the sufferer’s suspicion much more convincing than tales told by someone suffering from PPD or a psychotic disorder. A Borderline is generally imagining the worst about people and situations, because their imagination is unimaginably negativistic. Without being able to maintain integrated or realistic interpretations of others, a safety bias towards all things bad becomes their go-to conclusion. Untreated people with BPD often interpret non-personal commentary, innocent jokes, and neutral glances as potential forms of mockery because all incoming information from their surroundings is suspect. Of course, their imagination consistently gets them and others into trouble when confabulation replaces accurate appraisals. It could be said that people with this disorder are guided under unlucky stars by a here-be-dragons map. People with BPD confabulate events based on a combination of cognitive distortions, emotional convictions, unfounded biases, and lapses in autobiographical memory (experienced by others as pathological lying). They’ll demand loyalty to their narrative, but their narrative is usually inconsistent, exaggerated, or exceptionally wrong. For example, BPD paranoia produces an epistemological phenomenon known as discordant knowing, which is a cognitive framework that can make a person with this disorder highly susceptible to disinformation, conspiracies, and fanaticism. Unfortunately, paranoia further obstructs Borderline patients from developing introspection because focusing on factitious adversaries keeps most of their attention wrapped up in suspensefully distressing concerns.
It’s equally important to avoid misinterpreting Borderline defiance as a form of self-assurance or contumacious independence; it’s an expression of fear and frustration. The “edginess” that people with this disorder exude comes with a recurring tendency to drive themselves and others over the edge. Having a “cheeky attitude,” rebellious temperament, or flair for sarcasm is a defensive cover-up for morbid insecurity. People with BPD generally behave like militant cowards during adult confrontations; perennially afraid of others but highly potent when defending their fragile psychological territory. Likewise, destructive coping mechanisms learned in childhood are systematically incorporated to acquire various wants and needs. To be sure, giving a Borderline’s snarky proclamations the benefit of doubt will not benefit anyone, including themselves, but giving their feelings the benefit of the doubt provides much needed validation. Other misinterpretations may include believing the BPD to be a scapegoat (identified patient) of other “crazy makers” rather than investigating the patient’s contributions to their own psychosocial predicaments. To make matters more convoluted, Borderlines often expect professional relationships to be indistinguishable from personal relationships. Therapeutic relationships, in particular, are anticipated to become more intimate and time consuming because BPD patients need to be convinced that their therapist’s empathy and caregiving is unconditional. But whenever the lens is focused on them, Borderlines will interpret challenging clinical interactions to be a simulacrum of parental judgment by an authority figure with the potential for criticism and shame—even the therapist’s tone of voice can set off an adverse reaction in these uniquely hypersensitive patients. Subsequently, BPD patients will work hard to undermine the power differential by controlling the therapeutic process to avoid anxiety in the face of uncertainty. The process of change equals an all-too-familiar source of stress and unpredictability that subconsciously reminds them of their childhood. Overall, Borderlines prefer power over uncertainty rather than working towards self-actualized empowerment. They must win rather than reflect, because they see the world through the eyes of a scared and highly competitive child.
Immaturity can be seen whenever reality interferes with the Borderline’s need for validation, resulting in boredom and impulsive attempts to regain recognition, or whenever serious discussions require reciprocal engagement among adults. It’s more important for a person with BPD to control the direction of conversations than focusing on the substance of conversations. Therapeutic relationships are meant to be productive collaborations, but building a therapeutic relationship with a BPD patient has a much greater likelihood of becoming contentious or dependent because of their distorted perception of trust. Trust, from the Borderline’s perspective, is based on the acceptance and availability of the therapist to meet their needs. A good diagnostic benchmark is to pay close attention to the patient’s style of interaction. Excessive irritability or excessive congeniality are key indicators for ruling out Cluster B pathology. Borderline patients employ polarized attributions towards others (good object/bad object), and their affective presentations and beliefs about themselves are equally divided. Because people with BPD cannot accurately identify the source of their suffering, which makes them feel alone and like strangers in their own bodies, they desperately need others to identify with their pain.
“Borderline patients seem to have the peculiar ability to inflict a specific form of ‘sweet suffering’ on their therapists. They themselves have suffered throughout their lives, and it is important to them to have their therapists suffer for them. They seem to demand that the therapist abandon the professional therapeutic role so that whoever attempts to treat them must share in their misery,” states Dr. Glen Gabbard. Or, as Otto Kernberg once put it, “It is as if the patient’s life depends on keeping the therapist under control.”
It’s important for therapists to be prepared for anything in terms of complex behavioral dynamics and counterintuitive encounters with problematic patients, even if nothing can fully prepare them for the unique challenges they may face when attempting to treat a Borderline.
“While many psychological disorders can generate strong feelings in a clinician, few stir such intense reactions as BPD. Patients with BPD are also often viewed as difficult and provocative when compared to patients with other diagnoses. In a survey of clinical psychologists, a patient with BPD features was ranked the least desirable to treat when compared to someone with depression or schizophrenia. These attitudes towards patients with BPD probably impact their care. Private-practice clinicians may be reluctant to treat them and some evidence shows that public-practice clinicians limit services and decrease expressions of empathy for BPD patients. Patients with BPD typically evoke intense reactions within the therapist that can be difficult to manage. When the patient is distressed, the therapist often feels helpless, guilty, and pulled to rescue. When the patient is belligerent, the therapist often feels incompetent, angry, and pulled to retaliate. Patients who have BPD exhibit an uncanny ability to identify a therapist’s personal and professional vulnerabilities. Gabbard & Wilkinson (1994) argued that even experienced clinicians get caught in countertransference enactments. Comments about the beginning therapist’s experience, training status, and competence should be expected, as should appeals for more time after a session ends, physical contact, extra-clinical contact, and special privileges. Therapists may react in ways that are critical, collusive, hostile, passive-aggressive, seductive, symbiotic, rigid, rejecting, or blaming. Such reactions are associated with poor outcome,” according to Matthew Merced, Psy.D.
Love is a battlefield. — Pat Benatar
A Borderline’s history of romantic relationships is characteristically unstable and stormy. Likewise, there’s often evidence of intermittent reinforcement relationships that are intense, turbulent, and ephemeral. People with BPD are looking for someone to love and someone to blame to compensate for adverse childhood experiences with primary caregivers. As a result, BPD relationships are representational, dependent, and transactional rather than egalitarian and interdependent. Borderlines want the appearance of an adult relationship with the fulfillment of a parental relationship. In this sense, their concept of a relationship is pathologically immature. They’re unconsciously searching for an all-loving, all-caring, and all-giving surrogate parent. Consequently, the ambivalence they felt towards their parents will be projected onto their partner. This “hot and cold” relationship style is based on an approach-avoidance conflict (e.g., “I hate you, don’t leave me”). Borderlines also engage in paradoxical thinking that may alternate within minutes, hours, or days. Their positive emotions can make them irresistible to engage with, but their negative emotions quickly render them insufferable. Confusing and contradictory in its push-and-pull nature, this self-defeating dynamic can bring fast connection, enthusiasm, joy, and intensity to relationships, but it also creates a breeding ground for disappointment, anxiety, and hostility. It draws people in, but it eventually pushes people away. For Borderlines, their search for an idyllic version of love is a defense against feelings of fear, emptiness, contempt, loneliness, and self-loathing. Subsequently, love becomes a clinging form of desperation, saturated with jealously. Having a toxic relationship with themselves (intrapersonal) results in having toxic relationships with others (interpersonal). The grave assumption of the person suffering from BPD is that all relationships will or should resemble some variation of the pathogenic relationship they almost universally had with their parents, which means they’ll feel misled and mistreated by anyone who attempts to love them. The final outcome is being suspicious of a relationship that the person with BPD initiated with great enthusiasm until the endeavor is brutally sabotaged by their own misgivings.
Frank Yeomans, a New York City psychiatrist, describes those with Borderline Personality Disorder as failed romantics. “They seek an ideal of perfect love and pursue it zealously. But as soon as the people they’re besotted with are a few minutes late, or can’t text during a busy work day, BPD sufferers go into a tailspin.” A friend or lover is either “just perfect or all hell breaks loose,” he says. “The borderline mind has not yet been able to integrate positive loving feelings with negative ones, such as frustration and anger. Since every relationship includes a whole range of emotions, you’ve got to deal with all of it to have the relationship work out.” People with BPD exhibit a preoccupation with nurturing and reparenting under the guise of an adult romantic relationship as the solution to their problems. However, long-term pair bonding is extremely difficult with Borderlines because of their predisposition towards irrationality, fear, self-sabotage, age regression, paranoia, separation insecurity, and rage. More specifically, an inability to be emotionally subdued for any substantial period of time, and the inability to maintain a stable image of themselves and others (object/introject inconstancy), are chronic features in the BPD’s universe of fluctuating feelings. Bonding with a Borderline is fundamentally a sadomasochistic endeavor, because they devalue themselves to such an extent that devaluing their intimate partner becomes inevitable. *Intimacy for an untreated person with BPD prioritizes contact comfort to soothe psychological pain rather than intimate adult experiences based on healthy differentiation. Developing close connections through some type of relationship is their brain’s way of healing itself, but it ends up having the effect that paradoxical undressing has on a person dying from hypothermia.
According to psychotherapist Ross Rosenberg, “Their [Borderlines] romantic relationships begin quickly, intensely, and with a great deal of excitement, euphoria, and sexual chemistry. Their volatile emotions move in one of two directions: love and adoration or hate and destruction. Because this person has had little-to-no experience with healthy relationships, the euphoric ‘perfect love’ feelings that occur in the beginning of the relationship are neither realistic nor lasting. The early euphoric love experience is transient as their psychological fragility leads them to an eventual emotional crash and burn. This black-and-white approach to their romances creates a teeter-totter effect of extreme behavior; they either shower their partner with love and kindness, or rage at them with disgust and violence. Their love/hate processing of relationships places an impossible burden on the partner. Often individuals diagnosed with BPD are preoccupied with real or imagined abandonment, which they frantically try to avoid. The perception of impending separation or rejection can lead to profound changes in the way they think about themselves and others, as well as in their emotional stability and behavior. Whether real or imagined, any reminder causes them to strike back at their romantic partner with rage and aggressive hostility. A mistaken comment, a benign disagreement, or an expression perceived as disappointing can quickly transform their loving feelings toward their ‘soulmate’ into a raging retribution against an enemy.” When it comes to the liabilities of love, Borderlines are tortured souls who torture others by association.
“My clients with Borderline Personality Disorder tend to focus on finding true love as the solution to their problems,” says psychologist Elinor Greenberg.
Perhaps most unusual is the fact that a Borderline’s preoccupation with friendship, affection, love, and romance (features of intimate bonding that all humans desire) are also characteristics of their disorder. Consequently, Borderline Personality Disorder can present itself as an endearing value system based on impassioned convictions rather than a complex character disturbance. For a person with BPD, fixating on these lofty sentiments becomes a coping mechanism to attenuate anxiety, loneliness, emptiness, and the fear of abandonment. Many people who have been neglected do not know how to feel connected in a healthy way; consequently, the “love” they seek is obsessive love. Having no experience with being authentically or consistently loved during childhood, a person with BPD imagines what untainted love must be like and often seeks this ideal with uncompromising vigor (aka “love addict”). Of course, ideal love for a disordered mind is nothing more than idealization, and idealization is tainted love, best defined as limerence (obsessive infatuation). Furthermore, a Borderline’s capacity for healthy interrelatedness is disrupted by poor object relations and object inconstancy while being strongly correlated with traits for secondary psychopathy, especially during periods of significant stress. PCL-R Factors 2a and 2b indicate reactive anger, aggression, impulsivity, shallowness, difficulties in planning, irresponsibility, social parasitism, and a sense of entitlement. According to the Five Factor Model (OCEAN), individuals who are low in agreeableness, high in antagonism, and high in disinhibition tend to have insecure attachment, deficient caregiving, high neuroticism, high dominance, and unrestricted sociosexual orientation. Dominance in relationships, overtly or covertly expressed, ensures that the Borderline’s physical and psychological needs are met, regardless of their partner’s availability or well-being. To the extent that people with this disorder do not grasp the dynamics of normal social or intimate relationships has to be experienced to be believed. Borderlines essentially repeat toxic relationship patterns of all types without knowing what in the hell is going on between their ears, but each time it happens they hope something will be different. Caveat emptor: Deep in the woods of Borderlandia, hate eventually becomes a substitute for love, because love is an egocentric prelude to a much darker world where no void is capable of being satiated. It’s all peace, love, and understanding until somebody gets hurt.
“Borderline patients find it very difficult to tolerate being alone but are also exceedingly wary of others. Terrified of abandonment on the one hand and of domination on the other, they oscillate between extremes of clinging and withdrawal, between abject submissiveness and furious rebellion. They tend to form ‘special’ relations with idealized caretakers in which ordinary boundaries are not observed,” says Judith L. Herman, M.D.
Whether explicitly or implicitly communicated, an overwhelming desire to be saved from their traumatic history, emotional pain, dissatisfaction, loneliness, fears, and sinkhole of learned helplessness is how the gradient of coerced caretaking begins. Unfortunately, any willingness to accept such responsibility on behalf of the therapist is an ambush for disappointment and devaluation because no caretaker can realistically ascend to the Borderline’s idealization standards, mostly because the existential imperative to find an external solution to resolve internal conflicts and compensate for core deficits is not based in reality. It could be said that people with BPD are highly sensitive individuals except when it comes to how their litany of needs affect those whom they depend upon the most.
The brain is the organ of destiny. — Wilder Penfield
The neuroscience of Borderline Personality Disorder is both fascinating and unsettling. Borderlines interpret their surroundings through a gallery of uncensored emotions that defy normal comprehension, and their sense of self and others is grossly misaligned. Overall, BPD is the preeminent domain of irrationality. If people with BPD are victims of anything, they’re unquestionably victims of the internal mechanisms of a discombobulated mind. Remember, BPD is not just a relational-behavioral disorder; it’s a brain disorder. There are significant differences in both the structure and operational dynamics of the brain with people suffering from this disorder (early and chronic childhood trauma often interferes with neurocognitive development). Developmental features of the mind that most of us take for granted are generally absent, diminished, or in total disarray for people with BPD.
It’s well known that the brain’s limbic system—more specifically, the amygdala—generates the bulk of human emotions, including feelings of love, sexual desire, fear, aggression, and hatred. However, these emotional states are normally regulated by the brain’s prefrontal cortex to ensure continuity of experience within the parameters of external reality. Subsequently, an electrical storm of impulsive potential becomes as unpredictable as it is unmanageable for people suffering from affective dyscontrol. In some cases, the Borderline’s prefrontal cortex is structurally malformed with evidence of temporal lobe dysfunction. In addition, hippocampal atrophy and anterior cingulate reduction are often identified with overactive limbic responses, which results in mood swings, panic, and dissociative amnesia. For people with BPD, the fight-or-flight trauma response seldom takes a break due to their high index of suspicion. Borderlines are basically stuck in Jung’s warrior stage of development with the world’s hardest-working sympathetic nervous system. Excessive reactivity occurs when critical faculties are not functioning properly during periods of stress because Borderlines have weaker circuitry for inhibiting inappropriate reactions to negative emotions (low vagal tone). These “filters of reason” appear relatively absent or significantly diminished in Borderlines, thus resulting in a unique hyperarousal of the limbic network with unregulated feeling states. In addition, studies have shown that people with BPD have an overactive hypothalamic-pituitary-adrenal area (HPA axis), which creates hypersensitivity as manifested through excessive anxiety, suspicion, and worry. For the most part, emotional dysregulation is made worse by hormonal dysregulation (high levels of cortisol, vasopressin, testosterone, and noradrenaline), which intensifies fear, dysphoria, territorialism, and aggression.
When Borderline Personality Disorder is misdiagnosed as Bipolar Disorder, it’s crucial to understand the difference between cycles of mood caused by neurochemical instability (Bipolar) and mood lability or emotional instability arising from the influence or perception of stressful interpersonal factors (Borderline). To put it mildly, people with this disorder have a brain that reacts to stress differently than the rest of us. Consequently, a Borderline’s anger can go from 0 to 100 in a matter of seconds with poor amenability to de-escalation. From a mental health perspective, BPD is a limbic-dominant condition (hyperactive amygdala functioning and hypoactive cortex processing). Furthermore, when people with this disorder cannot express themselves or understand others easily, they quickly become frustrated and anxious. Subsequently, people with BPD will create a world that makes sense to them as a way of overcoming or compensating for cognitive impairments in the brain’s fronto-parietal network (FPN), hence primitive defense mechanisms and primitive drives for survival. On balance (pun intended), Borderline Personality Disorder emanates from a complex interaction between environmental, anatomical, functional, genetic, and epigenetic factors.
Because the Borderline’s feelings are not regulated by the brain’s usual gates and checkpoints, a wide range of competing emotions are experienced with incomparable intensity. For the observer, witnessing these extremes of emotion is both captivating and terrifying because people with this disorder can be unbelievably charismatic in one moment and sullen or spiteful in the next. Their feelings of joy, love, and enthusiasm are as unrestrained as their feelings of fear, paranoia, anger, hatred, and resentment. For example, euphoric displays of idealization and affection are compelling because such emotional intensity is abnormally exciting. Upon introductions, some Borderlines have an almost otherworldly effect on others due to their dynamic energy, disinhibition, and eagerness to connect. In fact, their positive emotions and sense of immediacy are often so hypnotic that it’s easy for anyone who comes in contact with them to lose reality testing. On the downside, disproportionate expressions of anger will be experienced by others as completely unexpected, vicious, unwarranted, and bizarre. Anger for people with BPD emerges from fear, feelings of betrayal, separation anxiety, frustration, and humiliation, but it’s typically curated by cognitive errors when assessing the motivations of others. Furthermore, an untreated Borderline’s emotional reactions during periods of extreme stress are not amenable to modulation or introspection due to dissociation, derealization, and depersonalization. In fact, these feeling states (self-states) erratically alternate without warning—as if the person is completely summoned by uncontrollable urges. Periods of paranoia and increased tension brought about by interpersonal stressors often precede acute emotional discharges that will launch a person with this disorder into a different persona, but the moment when this occurs is relatively unpredictable. Not having a cohesive sense of self results in shifting moods, emotions, perceptions, goals, plans, and values. Likewise, correctly interpreting the actions and motivations of others is next to impossible when the capacity for interpersonal integration is absent. As the Borderline’s mood runs amok, a backdrop of fear and catastrophizing becomes omnipresent—like an invading shadow that permeates everything.
The BPD’s manifest image is contingent on the precarious mechanisms of a reactionary mind, and this uncanny juxtaposition will surprise anyone who tries to make sense of such counterintuitive behaviors and cognition. As a general principle, Borderlines overwhelm others because they’re overwhelmed by their own emotions. Dysregulated minds are primarily self-serving minds, especially when reality threatens their hard-won defense mechanisms. Borderlines experience significant difficulty with cognitive empathy (understanding the perspective of others) and they exhibit “thin skin” when it comes to being offended or feeling hurt. Although they’re known for being able to “read” others via mental state discrimination, their empathic attunement is more akin to self-referential hypersensitivity; likewise, they have recurring problems correctly interpreting social cues, similar to what occurs with Autism Spectrum Disorder. Their significant capacity for emotional empathy is self-oriented rather than other-oriented due to infantile dependency needs and psychic equivalence (feelings become facts). Furthermore, emotional empathy is negated by emotional instability during stressful intimate interactions. In fact, empathic accuracy (cognitive empathy) is highly correlated with stable relationships, and untreated Borderlines can’t “do” stable relationships, partly because they personalize the dynamics of interrelatedness through a deviant self-referential process that’s negative, hypersensitive, and paranoid. The feelings of a Borderline are intense and sincere in each moment, but they lack continuity and are subjectively biased with an unhealthy dose of neuroticism. When the rubber hits the road, their reactivity can become so merciless that it will burn down everything just to restore a sense of safety. Overall, consideration for others and the consequences of their actions take a back seat to fear and rejection sensitivity. People with BPD often posses a variety of desirable characteristics and qualities of cognition, but they degrade, disappear, or backfire the minute you introduce the confounding variable of a relationship—the very thing they want more than anything. When they’re in an idealized relationship space, they feel happy and relatively stable; but a reality-based relationship space makes them feel paranoid, anxious, and avoidant. Unlike people with Narcissistic Personality Disorder and Antisocial Personality Disorder, a person with BPD will try very hard to approximate relational compatibility and embody concepts like devotional love by embracing platitudes, saying the “right” things, transforming themselves for maximum desirability, being circumstantially loyal, and instigating affectionate gestures. However, the tragedy is that the Borderline’s repeated failure to actualize their bespoke version of love will inevitably become the failure of their loved ones. To be sure, BPD is a “reason is a slave to passion” disorder.
*Caveat for therapists to consider: Borderlines are more responsive to emotional and physical demonstrations of care (i.e., proximal reassurance, comforting voices, hugs, smiles, and positive eye contact) than they are to logical conversations about the importance of behavior management, introspection, and developing self-efficacy. For the Borderline, sentiments of caring must be demonstrated by action on the part of the caregiver. However, too much openness on behalf of the therapist will be misinterpreted by a Borderline patient as absolute acceptance if it’s not tempered with an adequate amount of reasonable confrontation. People with this disorder also experience difficulty sitting still or being left alone for extended periods of time and may engage in a variety of eccentric behaviors to distract themselves from painful feelings. Furthermore, Borderlines sometimes believe that they can accurately read people’s minds, or believe that others should be able to read their minds based on unspoken expectations (people with BPD rely heavily on psychological projection to compensate for problems with social cognition). Difficulty in communicating the qualitative aspects of their inner turmoil is common, which results in more confusion for anyone who wants to help them. In such situations, the patient and therapist may feel like they’re talking past one another, when, in fact, they’re speaking different languages. These gaps in communication require therapists to understand the Borderline’s object relations dialect of the unconscious (transference) before attempting intervention. There are also non-mentalizing modes of processing and communication among Borderlines that must be understood to parse the internal and external dynamics pertaining to all clinical interactions.
Being a hero is about the shortest-lived profession on earth. — Will Rogers
Borderlines are like runaway trains searching for someone who will save them from another episode of emotional derailment. In their compulsive quest for control, they are literally out of control. People with BPD can surreptitiously condition others to respond to their feelings of desperation through forced teaming, and conscientious therapists may feel compelled to go the extra mile—like a case manager on steroids—as a gesture of loyalty. However, these expectations place enormous pressure on therapists to compensate for the patient’s desire for unconditional support. Unfortunately, countertransferential rescue instincts will only reinforce the patient’s dependence and further vindicate their assertions of distress (people with BPD often claim to be mistreated by those who are supporting them). Nonetheless, the therapist may feel obligated to take care of the Borderline until the caretaking fuel runs out. To be sure, a clinical death trap of Faustian proportions awaits the therapist if they become the patient’s go-to person (aka “favorite person”). The Borderline’s favorite person is based on a fabricated image (distorted other) that places the therapist on a superhuman pedestal to serve unfulfilled dependency needs. Because a person with BPD views their favorite person (FP) as someone they cannot live without, the life of their chosen stabilizer is expected to accommodate the mental topography of the sufferer.
A subset of people wit BPD reside in an elaborate fantasy world (paracosm) inhabited by heroes and villains to protect themselves from painful memories of childhood trauma. In terms of non-mentalization modes, this fantasist-inspired way of seeing oneself in relation to the world is called the pretend mode. As a consequence of such unrealistic constructions, therapists will unknowingly be subjected to tests and confirmations that either prove or disprove their caretaking worth within the patient’s internal fantasy structure. The Borderline is reflexively “fishing” for responses that ensure trust and safety from an “all-good” mother and reassurances that their perceptions are valid. Subsequently, the personification of a mythological trope ensues: The therapist, like so many before them, becomes the Borderline’s latest knight in shining armor. In this seemingly marvelous reconnaissance mission, the patient’s need to feel protected and nurtured matches perfectly with the therapist’s need to be seen as a compassionate and competent caregiver. Furthermore, effusive praise provided during idealization transference further incentivizes rescue responses. Unfortunately, the patient’s performance evaluation of the therapist’s valiance will undoubtedly result in massive disappointment under the encroaching weight of reality. There’s no perfect caregiver, and Borderlines must reconcile with this fact. Meanwhile, therapists should refuse to accept the nomination.
“Borderline individuals have a very interesting superpower. They can convince other adults that they are a needy child. Their ‘secret superpower’ involves putting out an energy that makes other adults want to take care of them,” states psychologist Elinor Greenberg.
From a research article entitled Understanding a Mutually Destructive Relationship Between Individuals With Borderline Personality Disorder and Their Favorite Person: “In most instances, FPs are friends, crushes, romantic partners, family members, or others with who the person with BPD interacts (teachers or therapists). When referred to as a FP, it goes beyond what other people would generally refer to as their best friend or favorite person. FPs are the object of complete attachment and extreme love from people with BPD. Therefore, those with BPD feel unable to function properly without their FP and fear that their FP will abandon them. Individuals with BPD are likely to have these relationships, in which the love they feel for their FP is all-consuming and so overwhelming that it is beyond their control; they often have no idea what they are doing toward their FP. In other words, FP is someone who a person with BPD is especially obsessed with even when they have other close friends; FP becomes exactly who the person with BPD needs at that moment.”
As endearing as all this may sound, there’s a hidden punchline with an emphasis on the punch: “The FP–BPD relationship often gets worse with time, as the person with BPD needs more attention and validation from their FP to get the same feeling of being cared for. Consequently, the FP faces more responsibilities and pressure to fulfill their person with BPD’s needs, such as constant contact. FPs are then highly likely to feel suffocated in the obsessive relationship, as they feel their boundaries are no longer being respected. They have to repeatedly comfort when their person with BPD suffers from the perceived abandonment, often to the extent that they feel unable to set healthy boundaries and function normally or socially, feeling the need to maintain a safe distance. Although they politely and cautiously try not to upset their person with BPD, it still strongly influences their emotions and behaviors. Those with BPD struggle with what is known as ‘splitting’ on their FP, constantly shifting between idealization and devaluation; the shifting goes between these two extremes. When they are in the idealization phase, their emotional attachment toward their FP is strengthened. However, when their FP fails to fulfill their expectations, they are immediately devalued, causing anxiety and depression, sometimes anger and panic attacks. The relationship gets to the point where it stops being a good friendship and turns toxic and destructive. Those with BPD can get too reliant on and obsessed with their FP to get out of the relationship but the emotions they experience, simultaneously, are too intense to stay secure and healthy in the relationship.”
In many ways, the uninformed guardian of the Borderline, professional or otherwise, becomes Aristotle’s “Tragic Hero” whenever they succumb to Rescuer Syndrome. According to Aristotle, misfortune is visited upon the tragic hero “not through vice or depravity but by some error of judgment.” Due to their extreme dependency needs, becoming a Borderline’s favorite person is capital punishment for independent personhood. Like a light switch, their favorite person will inescapably become an abusive enemy who can’t maintain the dependency agreement, thereby justifying victimhood and the search for a new favorite person.
Nowhere is there warmth to be found, among those afraid of losing their ground. — Harold Eugene Clark
Because the most significant goal of untreated Borderlines is to gain the unequivocal concern of caregivers to compensate for abandonment wounds incurred by their original caregivers, this disorder may represent the most challenging condition for clinicians to work with when it comes to maintaining professional boundaries. For example, immaturity and separation insecurity causes people with BPD to interpret adult boundaries as a message of rejection—a reiteration of inherent unworthiness. In this sense, a boundary, no matter how reasonable or lenient, becomes the symbolic representation of micro-abandonment. As someone who lives in fear, a person with BPD is most afraid of losing their sense of control. “Staying in your lane” is antithetical to a Borderline’s need for external approval because they cannot generate feelings of self-acceptance. Like an addict, a person with BPD could be thought of as being addicted to safety, control, reassurance, recognition, regulation, and whatever denial is necessary to defend against an erosion of emotional supply. To get their “fix,” they must find a partner in crime, or situationally amenable circumstances, to secure these elusive safe-space conditions that are forever vulnerable to being obliterated by the hammer blows of reality. A boundary to a Borderline is a blockade against what’s needed to survive, even if breaching it potentially compromises everyone’s ability to thrive, especially when frantic attempts to avoid real or imagined abandonment become more frantic than any boundary can withstand.
Borderline Personality Disorder embodies a strange inversion of reasoning. People with BPD are aggressive and insecure; demanding and implacable; needy and suspicious; helpless and controlling; competitive and fearful; affectionate and contentious; fragmented and solipsistic; suggestible and resistant; fragile and combative; impulsive and apprehensive; entitled and self-effacing. Every trait is contradicted by another trait until the person suffering from the disorder is left feeling empty, anxious, angry, scared, lost, resentful, and alone while their significant others are left in a state of disorientation and disbelief. The Borderline is perplexed and tormented by the frightful discontinuity of their mental processes; everything is a potential crisis and everyone is a potential threat until proven reliable, but “proof” is unattainable due to the capriciousness of object inconstancy. Therapists have a job that depends on building trust with their clients, but BPD patients live in a perpetual state of mistrust. Impossible standards of care will be expected before the Borderline feels comfortable enough to temporarily trust their caregiver. However, attempting to fulfill these expectations is the beginning of an extraordinarily unusual and unsettling downward spiral.
In the world of BPD communication, everything is upside down and contradictory; it’s a complicated game of surreal semantics that must be carefully unpacked and methodically analyzed. Assumptions are dangerous. Words like trust, relationship, friendship, family, love, soulmate, and care have different meanings for Borderlines, and any deviation from their emotionally challenged dictionary quickly spells trouble. An overemphasis on heartwarming expressions that signify closeness serve to minimize separation anxiety (untreated people with this disorder do not understand the concept or importance of separation-individuation). Most importantly, affectionate phrases that galvanize proximity are not collaborative because Borderlines must control the dynamics of their chosen associations. No matter how synchronized you may feel when conversing with a Borderline, you’re not reading from the same page, chapter, or book. BPD speak is the coded language of trauma that passes as common parlance. Borderlines are relationally illiterate, communicationally challenged, interpersonally mistrustful, and emotionally volatile. There’s no intersubjective agreement because Borderlines—being low in agreeableness—expect others to agree with their distorted views regarding the nature of reality. Every mental health practitioner would benefit tremendously from attending Cluster B language school.
André Breton pointed out in the Surrealist Manifestos that the European tradition of enlightenment could not prevent the horrors of war. In a similar vein, Winston Churchill famously quipped, “You cannot reason with a tiger when your head is in its mouth.” Borderlines are the temperamental tigers of mental health patients; they have majestic stripes but a ferocious bite when they suspect criticism or rejection. Whenever the purring stops, there’s no headroom for negotiation or mulligans on the back nine. The Borderline’s reprisal-ready incisors are a custom fit for gullible caregivers who will go from being heroes to zeros if they rely on empathy and reason without incorporating a sizeable portion of precautionary intuition.
Givers need to set limits because takers rarely do. — Rachel Wolchin
“Setting limits with individuals with Borderline Personality Disorder often causes them to experience frustration which may be expressed as rage. Refusing them or restricting them in any way causes them to feel slighted, or worse, rejected. These feelings leave them feeling victimized, which then justifies lashing out behavior. This may take the form of challenges to the boundary, or possibly abusive behavior towards you for setting the boundary. Individuals with BPD not only feel the sense of helplessness that others associate with feeling like a victim, they also experience the boundary as an accusation of unworthiness,” says Dr. Daniel S. Lobel.
Borderlines crave the sensation of control, so therapists should expect to feel dominated at some point during the therapeutic process. People with this disorder repeatedly attach their well-being to preconceived outcomes that are typically inchoate and poorly communicated. Whenever these expectations fail to materialize, or fail to materialize according to the Borderline’s quixotic specifications, erratic thoughts and behaviors are likely to emerge. Therapists may rationalize exceptions to treatment and loosen boundaries by surrendering to the patient’s increasing demands to demonstrate solidarity within the therapeutic relationship. BPDs instinctively perceive boundaries as a form of neglect, so they’ll often ignore these inconvenient barriers to bonding. It’s a precarious predicament, because Borderlines think of themselves as being entitled to customized experiences that cater to their immediate emotional needs. Why shouldn’t they? After all, they feel numb, empty, bored, and worthless without a continuous supply of affirmation, consolation, support, and stimulation. Mental health patients who travel along the Cluster B bypass are no fans of delayed gratification. People with BPD fail the Stanford marshmallow experiment because indulgence supersedes forward thinking. For example, Borderline patients often expect frequent contact with their caregivers via phone calls, email, texts, and emergency visits. However, not wanting to alienate or hurt their feelings in the short term will result in confusion and resentment for both parties when boundaries are no longer amenable to remediation. For example, if therapy progresses from being professional to becoming more friendly, it’s only a matter of time before a BPD patient will initiate further efforts to decimate the remaining power differential. Shared decision making with a Borderline is treacherous territory because they want everything to reside on their turf.
The BPD’s urgency to have their needs prioritized can lead to multiple role endorsements by caregivers, such as becoming a legal advocate, family interventionist, apologist, avenger, secretary, friend, surrogate parent, emotional support pet, ambassador, chauffer, babysitter, punching bag, and emergency manager. It must be understood that Borderline patients will evoke strong emotional responses from their caregivers, and these responses are commonly experienced by therapists as intensified concern (i.e., feelings of pity, outrage, helplessness, or moral panic). For the therapist, being aware of their own emotions is just as important as being aware of their patient’s emotions. Therapists must trust their professional instincts more than the emotionally driven impulses of a person with BPD, but patients in distress can be difficult to assess with neutrality. Precipitously, the dynamics of therapy could be governed by the patient’s capricious emotional states instead of being effectively analyzed and redirected by the therapist. Borderlines are in the molding business as they search for those who are willing to become malleable acolytes in service of their “id without a grid.” According to psychologist Elinor Greenberg, the BPD’s basic message is: “If you care for me, you will do something to make it better right now!” The therapist’s protective instincts will automatically be innervated by such displays of desperation, because no caregiver wants to be seen as uncaring. For the love of god, will someone step up to the plate and please help this poor soul? It’s a Catch-22 situation. Like the parable of Thales, therapists can fall into a bottomless well of boundary violations by attending to their patient’s constellation of insurmountable needs. What was once an analytic space is now lost in space.
From an article in PsychCentral entitled, Why Do Therapists Stigmatize People with Borderline?: “It’s the ever-changing and very intense emotions that set someone with BPD apart from others. Their relationships are fast, furious and fleeting. Whether it be a friendship or a professional therapeutic relationship, people with BPD often find it difficult to hold on to it. Their thoughts are often characterized by what cognitive-behaviorists term ‘black-or-white’ or ‘all-or-nothing’ thinking. You are either 100% on their side, or you are actively against them. There is little in-between. Given this manner of looking at the world, it’s no wonder people with borderline personality disorder can be challenging to work with. They will often ‘test’ the therapist who works with them, by either engaging in impulsive, dangerous behavior (needing to be ‘rescued’ by the therapist, such as committing an act of self-harm), or by pushing the professional boundaries of the therapeutic relationship into forbidden areas, such as offering a romantic or sexual encounter.”
Psychotherapists face an unavoidable paradox. They must immerse themselves in the moment to empathize with patients and emotionally distance themselves to maintain boundaries, or offer perspectives to foster change (Bateman & Fonagy, 2006). Philosophically, therapists strive to adopt a dialectical stance in which they simultaneously accept the patient while facilitating change in the patient (Koerner, 2012). From a practical standpoint this means switching between validation and change during a session, often in the same intervention, and flexibly navigating this contradiction (Koerner, 2012). Gabbard & Wilkinson (1994) argued that therapists typically react by becoming either over-involved to “save” the patient or under-involved to emotionally distance themselves.
Controlling my environment was still a compelling need for me. I did everything I could to not be surprised by anything. Looking back, I think that my need to predict how my day was going to unfold was a direct response to the amount of chaos in my childhood. — Olga Trujillo
It’s important to be aware of the Borderline’s unrealistic expectations for validation, proximity, and reassurance. They cannot tolerate being alone (autophobia) and have great difficulty managing emotionally stressful situations. Without self-acceptance, people with BPD rely on acceptance from their environment to regulate their self-esteem. For example, Borderlines will instinctively identify characteristics in others, such as generosity or agreeableness, to get their emotional needs met, appearing retrospectively as premeditated manipulation. Incidentally, the longer a person with BPD has gone undiagnosed and untreated, the more refined their survival mechanisms will become. In layman’s terms, Borderlines are less interested in change than changing others to get what they need (alloplastic adaptation). Other people (need-gratifying objects) are in a position to provide special services, but if those services fail to meet their expectations, calamity will ensue. Therapists, by definition, are trained to be of service to those in need; however, BPD patients will take advantage of every accommodation offered while cataloging susceptibilities for future interactions. They will subjugate challenging interpersonal encounters because it makes them feel uncomfortable. For the Borderline, spatial distance may also be perceived as a sign of rejection. People with BPD simultaneously seek and reject help, because accepting help that requires emotional labor, experiential honesty, and courageous introspection makes them feel out of control. Notice the inherent contradiction: A helpless victim who needs to be in control.
Perfectionism, a common Borderline attribute, is another manifestation of control that acts as a substitute for external validation (“when I’m perfect, then I’ll be loved” or “I try so hard to be perfect, so why does everyone hate me?”). Because Borderlines were often raised in families where acceptance was based on performance, they will try to prove to the world that they’re flawless by conveying an image of competence, beauty, or success. Likewise, many people with BPD were expected to be perfect and compliant to win their parent’s approval, or to avoid punishment, so they’ll inevitably expect perfection and compliance from others (this is why Borderlines can be extremely judgmental and unforgiving). Counterintuitively, perfectionism also serves as a form of self-invalidation, as unrealistically high standards become self-imposed forms of psychological torture. Borderlines live with an embedded sense of “badness” that is often caused by insufficient mother-infant attachment and neglect, so they must punish themselves and/or others for perceived mistakes. It has been argued that BPD perfectionism symbolically represents a form of “emotional cutting.” In fact, many Borderlines experience somatic symptom disorders that are exacerbated by self-inflicted injuries meant to punish themselves or to alleviate tension and feelings of emptiness. To become the reification of perfection is meant to distance a Borderline from their trauma, but it also perpetuates it.
Inflexibility runs in tandem with perfectionism. Borderlines are perfectly content with letting the perfect be the enemy of the good. Things must go a certain way, and any sudden change in plans is anathema. The Borderline lives in fear, but control makes them feel safe. People with BPD will try to obtain as much control and power as allowed in adulthood to compensate for the lack of control they experienced in childhood. Control of their image and their environment is the Borderline’s primary method for fear management. What others think of them means more to a person with BPD than what they think of themselves. Meanwhile, they’ll dispatch a decoy of ineptitude as they demand unreasonable levels of support from anyone who gets too close, thereby exposing their emotional dependency. As a result of appearing victimized, the BPD’s concerns are often misinterpreted as legitimate complaints rather than pathological patterns of learned helplessness. Monopolizing the compassion of others is a full-time job. With Borderlines, you cannot separate personal motivation from pathology; it’s a distinction without a difference. Consequently, therapists who accept their patient’s assertions of helplessness at face value are headed for an imminent clinical disaster. *There’s a tendency to simplify treatment approaches when interacting with someone suffering from this complicated disorder because the patient’s stated concerns and symptoms may initially appear transitory rather than pervasive. The BPD’s victim identity can create an instant connection with caregivers, but this attachment is unrealistic and unendurable. Subsequently, therapists will lose objectivity if they allow themselves to become emotionally invested in their patient’s eternal quagmires. Welcome to the sunk-cost fallacy for therapists. A therapist can offer sanctuary to a Borderline, but they cannot protect a Borderline from themselves. Safe is one thing; sound is another.
Listed below is the Borderline’s “Tyrannical Toolkit” for obtaining recognition, affection, resources, and allegiance from family members, friends, romantic partners, professionals, and caregivers. Without healthy communication or coping skills, people with BPD take a “whatever works” approach to getting their needs met. Commanding the will of others is their primary goal to mitigate insecurities, anxiety, and fear of abandonment. Weaponizing emotions is the wheelhouse of the emotionally unstable. These survival-based methods for achieving control are strategically effective in the short term because they demand immediate responses from the Borderline’s favorite person, “target,” or intended audience, but they inevitably perpetuate a vicious cycle of relational sabotage.
When they discover the center of the universe, a lot of people will be disappointed to discover they are not it. — Bernard Bailey
Borderlines share many similarities with those suffering from attention-deficit disorders, but mostly because they believe that not enough people are paying attention to them. Most people with BPD were not validated in childhood as a consequence of parental neglect, so they’ll over-compensate for this lack of developmental stimulation in adulthood. In fact, emotional neglect due to growing up in an invalidating environment may be the most influential variable in the development of BPD. Attachment theorists have suggested that the route of continuity from infancy to adulthood is through the individual’s internal working model or schema of the relationships between the self and others (Ainsworth, Blehar, Waters & Wall, 1978; Bowlby 1969/1982, 1973, 1980; Bretherton, 1985; Main, Kaplan, & Cassidy, 1988). Like an angry infant in its crib, the Borderline will aggravate others until they’re fed. The baryonic matter of the cosmos must revolve around the Borderline’s gravitational force, but the total mass-energy is no match for their negative energy. This is why people with BPD are often described as selfish, bossy, theatrical, entitled, and impatient (aka “main character” syndrome). They’re on an unconscious mission to course correct for childhood deprivation, and they expect others to be complicit with their needs for recognition, reassurance, security, and love. For example, Borderlines who significantly overlap with histrionic and narcissistic pathologies will try to fill their emptiness with a continuous reinforcement of narcissistic supply (a pathological or excessive need for attention or admiration from others, or such a need that does not take into account the feelings, opinions or preferences of other people). Egocentric behavior is generated by fear, but sensation-seeking behaviors to “medicate” anxiety ironically result in more self-centeredness. Consequently, the behavioral trajectory of BPD is to win a Pyrrhic victory that supplies attention through drama and chaos. This need for centrality comes from a transactional message by the Borderline’s original caregivers: Attention is provided when the child is sick, in pain, or miserable. As with Munchausen syndrome and other factitious disorders, to manufacture a crisis brings attention to the creator. Furthermore, special attention in toxic families is usually received for any performance that reflects well on narcissistic parents. Subsequently, seeking recognition from others is how Borderlines regulate their self-esteem and circumvent loneliness. However, this chronic need for emotional fulfillment places extensive pressure on caregivers and is only made worse by appeasement.
Therapists often report feeling as if they have no life outside of their most demanding Borderline clients—there’s no division between their professional and personal lives. For example, there have been reports of BPD patients feeling abandoned if their therapist goes on vacation, gets sick, or becomes pregnant. It must be emphasized that Borderlines experience others in relation to how every interaction affects them. Because they’re hypersensitive and paranoid, conflict arising from minor misunderstandings is often inevitable. Conflict is not created for purposes of effective problem solving; it’s created to keep the spotlight on the Borderline’s emotional pain. Although people suffering from BPD describe attention-seeking behavior as a coping mechanism, which is clinically accurate, the end result commands the attention of others in a way that resembles premeditated manipulation. As with all parsing of BPD semantics, it’s another clinical distinction without a practical difference. Validation is an addictive drug for Cluster Bs, but the side effects are not limited to the user. “People with BPD often derive their sense of worth from how much other people are serving them,” says psychologist Daniel S. Lobel.
Harboring enormous levels of self-doubt, Borderlines experience a sort of “prosopagnosia of the soul” and rely on others to provide them with a sense of self and self-esteem. People with BPD are perpetually simmering in a rice cooker of self-loathing, anxiety, and loneliness. Otto Kernberg, a psychiatrist who pioneered a new understanding of Borderline Personality Disorder, believed that pervasive feelings of loneliness and the need to belong to something were the driving forces behind all of the other behaviors associated with BPD. For the Borderline, other people become props to help them achieve emotional stability while quenching their thirst for propinquity. Power through control over intimate others is their primary objective to avoid rejection and abandonment. Therapists learn that successful therapy requires patient engagement by developing a strong therapeutic alliance, but too much engagement with Borderlines will create an avalanche of unrealistic expectations. A patient with BPD is less likely to pay attention to the substance of therapeutic conversations because they’re usually focusing on details related to the interaction (i.e., the therapist’s tone of voice, eye contact, the appearance of the therapist, and other nonverbal communication cues). In other words, listening comprehension is secondary to the Borderline’s need to take inventory of their surroundings. Similarly, emotional preoccupations cloud their capacity for being fully present (people with BPD primarily exist in a dissociative state). Nonetheless, Borderlines are equal-opportunity seekers whenever emotional propitiation is on tap. For example, if the therapist has been showered with attention, this is because the patient is seeking validation for themselves. Compliance with the fanciful expectations of the disordered is expected, but don’t expect them to comply with the rules and expectations of others. Up is down and black is white. Over time, trying to navigate such duplicity will become overwhelming (discrepancy identification is a good heuristic for determining if a mental health patient is hitting home runs in the Cluster B ballpark). A Borderline will rely on their therapist as flotation device, but the water they’re drowning in is deep, opaque, and brimming with uncertainty. BPD patients often assume that caregivers should be available on short notice to eliminate their feelings of desolation and to soothe their anxiety. However, their hypersensitivity to criticism and lack of trust makes therapy exceptionally challenging without activating an inferiority/superiority complex (vulnerability switching into grandiosity). Every interaction is on a self-referential loop following a protracted path of self-interest and self-preservation. Because the therapist of a Borderline represents both an intimate other (parental figure) and an authority figure (object of disdain), the risk of clinical calamity is more likely to occur than with other mental health patients.
Borderline pathology overlaps with covert narcissism (aka vulnerable or “shy” narcissism), and narcissism thrives on the allegiance of others to avoid narcissistic injury. In addition to sharing the same cluster of disorders, the psychiatrist James Grotstein offhandedly referred to people with BPD as “failed narcissists.” Despite the diversity of their primitive defense mechanisms, they couldn’t make the cut in the pantheon of big league grandiosity. However, this “failure” is replete with many spectacular trial runs driven by their sense of entitlement. Although Borderlines often present as warm and friendly, their fear of rejection can trigger a level of compensatory grandiosity normally reserved for Narcissistic Personality Disorder (BPD and NPD comorbidity can exist). However, there are important differences that must be recognized between BPD and NPD. Narcissists are more “solid” in their defensive projections, whereas Borderlines oscillate quickly in relation to feelings about themselves and others with a significant fear of abandonment. Borderlines are primarily dysregulated, and Narcissists are primarily grandiose. Borderlines are predominantly searching for stability and safety, whereas Narcissists are searching exclusively for narcissistic supply (often obtained through status). Borderlines fear abandonment, and Narcissists fear vulnerability. Borderlines are prone to self-injurious behavior during emotional decompensation, whereas Narcissists prioritize their self-appointed physical and mental superiority. Narcissists exhibit grandiose/fearless dominance during interpersonal encounters, whereas Borderlines demonstrate a peculiar type of neurotic dominance that coincides with their approach-avoidance relational style (anxious but demanding). Nonetheless, the Borderline’s obsessive focus on how everything and everyone affects their feelings, or how every interaction is meant to be taken personally, places them along the narcissism spectrum in terms of morbid self-absorption (such solipsistic preoccupations epitomize a precarious type of egocentric neuroticism). Abandonment rage itself denotes inflated feelings of self-importance, wherein one cannot be refused. Likewise, paranoia delineates being the special subject of ongoing persecution, as if everyone is spending all their time plotting against the person with BPD. Furthermore, a common overemphasis on image management and perfection signifies “redemptive vanity” as a protective buffer for unspoken insecurities. Ironically, some people with BPD will accuse anyone who isn’t adequately focusing on them of narcissism, especially if there’s a diminution of appeasement from their favorite person.
“Live and let live” has no place in Cluster B weltanschauung, and their need for centrality is beset by a recurring sense of entitlement. Controlling others to satisfy internal regulatory needs encapsulates the crux of these disorders, and the extemporaneous nature of interpersonal differentiation causes severe stress because independence is interpreted as a threat to existence. In this sense, all relationships with untreated Borderlines are narcissistic relationships because the onus is on the non-disordered person to conform to the sensitivities and bottomless needs of the disordered. Likewise, rejection sensitivity causes some people with BPD to become reactively self-centered in a manner that would make a pathological narcissist blush. Therapists who aren’t suspecting Cluster B shenanigans will eventually be caught by surprise—like an off-duty police officer during happy hour—whenever they say or do something “wrong.” Deviations from the Borderline’s shifting expectations and unyielding standards are the equivalent of betrayal, and betrayal is abandonment with wings. If you try to fly away from a person with BPD on your own terms, they’re likely to make sure that your most serviceable feathers get plucked.
It is the fool who thinks he cannot be fooled. — Joey Skaggs
There’s a story my father told me about a man who was killed late one evening by a car with one headlight because he believed it was his friend on a motorcycle. Eager to greet his companion, the man walked into the middle of the street, only to meet his fate by the other headlight, moments before midnight. Self-deception is dangerous, regardless of our enthusiasm for something to be other than what it really is. Whenever presented with an incomplete image, our minds tend to fill in the dots according to what we want to believe (perceptual restoration) rather than what we need to understand before making assumptions.
Narcissists, anti-socials, histrionics, and borderlines (Cluster Bs) survive in large part by learning how to disguise their pathologies (near normalcy) in the company of others. After all, if people with personality disorders went around saying, “I have a pervasive mental disorder that makes me extremely difficult to be around,” they wouldn’t, at least according to Duke Ellington, “get around much anymore.” Humans are social mammals and life is a contact sport that requires various degrees of cooperation, so people with personality disorders must use what they have to get what they need. Borderlines, in particular, will modify their behavior, interests, and appearance to please others because they struggle with identity disturbance. Although everyone exhibits different sides of themselves according to various social circumstances, there’s a significant disconnect between how people with BPD they see themselves, how they want others to see them, and how they feel about themselves in relation to others. As if this ontological quandary wasn’t daunting enough, objective introspection is customarily missing from the equation and is made worse by poor social cognition. The Borderline’s shape-shifting capacity for presenting themselves in a carefully assembled manner is a survival-based façade (“false self”) that facilitates social acceptance while appearing normal, thereby distancing themselves from their traumatized core. In this sense, Borderline Personality Disorder is a Potemkin pathology that engenders prima facie interactions with others, and their ability to maintain composure through suppression can prevent or indefinitely postpone diagnosis. A relational rendition of Rene Magritte’s The Treachery of Images comes to mind: This is not a copacetic person; this is the image of a copacetic person (the Borderline’s false self gives the false impression that everything is in good order, but nothing could be further from the truth). The Borderline’s “shadow self” is a wrecking ball obscured by a glorious garden sculpture. Overall, people with BPD are highly skilled performers in need of a supportive audience to regulate the ominous vicissitudes of their inner landscape.
Borderlines can be captivating, energetic, seductive, and glamorous (especially predominant among those with histrionic traits) with enough élan vital to entertain a Roman auditorium. They’ve often been described as adventurous, fun-loving, “bubbly,” and free spirits by those who encounter them under favorable circumstances. There’s never a dull moment in Bordertown. They live for the moment, but they’re not fully present. Borderlines are very dynamic people, but it’s a brand of dynamism that’s not suitable for the faint of heart. Many Borderlines are creative and intelligent with interests that quickly become obsessive, but they can also lose interest just as quickly due to their impulsive, mercurial, and unappeasable character. Carpe diem is their modus operandi whenever elation reaches critical mass, but scorched-earth policies are not far behind whenever they feel disrespected, hurt, or rejected. Borderlines are very passionate and affectionate people, but it’s a passion propelled by pathology and percolating with unease. Not being allowed to individuate or express themselves during childhood, people with BPD will work hard to become someone whom they believe others will admire. In fact, Borderlines will generally work hard at any activity that provides them with a sense of control, order, validation, and completion (BPD determination should be bottled and sold on the black market). Their goal is to avoid feeling flawed, invisible, or inadequate by portraying an idealized version of themselves through appearance, possessions, or externally validated accomplishments. When image is everything, you’re interacting with a person who has learned to survive through uncompromising single-mindedness, presentation management, and mirroring better than a method actor.
Many Borderlines are known for their sultry sensibilities, sartorialism, and effortless ability to command the attention of others. Because their inner experience is feeling like they don’t exist, extraordinary efforts are made to obtain positive affirmation from society and loved ones. For example, BPD males commonly present with a hyper-masculine persona that exudes bravado, whereas BPD females often present with a hyper-feminine persona to offset core insecurities. From the damsel in distress to the femme fatale; from the forlorn cowboy to the rebel without a pause. Regardless of the particularities of posturing, the underlying fabric of this disorder is woven from the fragile threads of what’s idiomatically referred to as Peter Pan syndrome and the Cinderella complex. BPD is a lifelong search for parental approval while ultimately being afraid of the adult world and its disconcerting vicissitudes, which is why people with this disorder resemble lost children, oversensitive toddlers, and troubled teenagers. Borderlines want to be noticed, accepted, and thought of as desirable, but yet they resent being objectified. Ironically, their loved ones become need-fulfilling objects (object-representation other).
Overall, people with BPD are known to be attractive in appearance and appealing for the intensity they bring to their pursuits. However, therapists must learn to ignore the patient’s window dressing (supernormal stimuli) and pay closer attention to how the furniture is arranged inside the building. In other words, therapists must be good at reading between the borderlines. The false self is a protective form of misrepresentation; an eminence front; an imaginary friend; a constructed persona; an empty vessel posing as a packed cathedral. Underneath their veneer of well-crafted pageantry lies a cauldron of festering resentment, fear, and insecurity from unprocessed frustrations. A person with BPD may also change jobs, clothing, partners, friends, hobbies, living locations, or the color of their hair to fill the emptiness within, but these “changes” are superficial and ultimately dissatisfying. To hide behind something external is to avoid what’s hiding inside. The belle of the ball is providing cover for a shambolic rageaholic, and the rogue adventurer is secretly harboring a bête noire. Without warning, the helpless and innocent butterfly can become a paranoid and vengeful grizzly bear. For therapists who received the memo, they must find a way to respect the person without respecting their defensive costume. Taking the false self seriously encourages denial, but falsity of self is not always apparent (the bigger the trauma, the better the wrapping). A Borderline’s appeal, because most people with this disorder are unequivocally intriguing, is both an asset and a liability in terms of fostering insight. For example, it’s difficult to resist enabling a person with BPD because they respond so elatedly to anyone who offers help, but this also keeps them from examining and overcoming pervasive patterns of dependency. Their openness to experience and eagerness to connect makes them easy to talk to, but being low in agreeableness and high in reactivity prevents emotionally challenging conversations. Borderlines are hard not to like on the upswing, but they’re also harder than nails when it comes to peeling away their polished exterior.
Borderlines covet the relaxed confidence, happiness, and healthy autonomy of others (a source of endless curiosity and envy). Why can’t they feel like that? Pretending to be well-adjusted is an act that has a very short shelf-life, but their tenacity for approximation is remarkable. Sadly, Borderlines rarely believe good qualities about themselves, no matter how much others believe in them. Ironically, people with BPD generally dislike themselves and can’t believe anyone would really like them, but they can initially come across as some of the most likeable people you’d ever encounter. Occasional bursts of arrogance are quickly subsumed by fear, and their potential for winning over audiences is repeatedly snuffed out by self-sabotage whenever they internalize or externalize their aggression. Despite their propensity for compensatory grandiosity, the valence of Borderline Personality Disorder is perennial desperation. Reassurance-seeking is the Borderline’s raison d’etre, and it’s the most obvious warning sign of morbid insecurity. To act in desperation suggests a need for protection, although vulnerability among Borderlines is seldom revealed as a form of psychological subterfuge that subsidizes their illness. The narratives given for their behavior may appear reasonable until their patterns are discovered, because Borderlines don’t know who they are, why they feel like they do, or why they do what they do.
According to psychoanalyst Donald Winnicott, there are five degrees of the false self. In the worst-case scenarios (extreme pathology), the true self is completely hidden. The false self is required to become so strong that it appears to be the true self. To be sure, people with BPD are much easier to recognize when their suffering results in destructive behavior or visible disability (i.e., overwhelmed and unable to function). At the other end of the scale, the “nearly normal cases” still retain a false self but are able to meet ordinary social expectations. Basically, the Borderline’s suit of armor has expired but they refuse to shed their safety blanket. However, once their false self begins to crack under stress, an impressive display of defensive reactivity will light up the night sky. Keep your eyes on the powder keg; avoid being blinded by the smoke, and beware of the fireworks. To paraphrase Thomas Dolby, they’ll blind you with defiance.
*Borderlines often place themselves in double binds based on pervasive patterns of self-sabotage; likewise, they’ll incorporate double binds to acquire unambiguous commitment from caregivers. These no-win situations are efforts to preemptively avoid abandonment, but they’re often presented as cordial offerings that caregivers would be considered impolite or cruel to refuse. Borderlines crave stability and safety like a live wire requires neutral sources for proper conduction, so they’ll poke and prod to find out what their therapist is made of. Any response is better than no response to a person with BPD, but the “right” response is adjudicated by the caprice of their needs. Some mental health patients are pejoratively described by the psychiatric community as “med seekers,” but Borderlines could easily be described as “people seekers.” To regulate their emotions, Borderlines need people like diabetics need insulin. More specifically, exclusivity in relationships diminishes feelings of emptiness and aloneness. However, the patient’s fragmented identity is a foreboding challenge for therapists who haven’t been properly trained in treating this condition. The monumental task of restoration through integration (rupture and repair) is difficult to address without producing anger or enmeshment. Too little engagement results in accusations of not caring, and too much engagement reinforces dependency. People with BPD have a preternatural antenna for spotting others who appear approachable and charitable, such as non-confrontational caregivers or codependent types who are committed to fulfilling the needs of others. To reduce anxiety caused by ambiguity, Borderlines may work to create an atmosphere of friendship via forced merriment. As a result, the therapist’s temptation to become more amicable and accessible may allow an undiagnosed Borderline to avoid being confronted in crucial ways that would ultimately reveal their disorder. Psychotherapy stirs up a lot of emotionally painful subject matter, and BPD patients will find clever ways to shut it down by using whatever defense mechanisms they have at their disposal. Nonetheless, having the courage and energy to follow the Borderline’s evasive trail of denial will inevitably lead you to their unresolved emotional wounds.
Fool me once, shame on you. Fool me twice, shame on me. Fool me three times, and you’ve probably developed a characterological disorder that has been fooling everyone, including yourself.
Voices carry. — Amiee Mann
Too much self-disclosure is potentially dangerous when working with BPD patients. The therapist’s efforts to relate to their client may result in revealing information that will eventually be used against them. A Borderline patient will eagerly commiserate with their therapist, but they’ll also commiserate with others about their therapist. Although Borderlines despise equivocation and prefer direct communication, transparency is a double-edged sword that will hang over the head of a therapist like a guillotine. Most therapists do not have the power of prescription. What do they have? The power of conversation, encouragement, reassurance, empathic relatedness, and emotional support. However, the very qualities that make therapists good at what they do (i.e., attentiveness, compassion, consideration, empathy, respect, and accommodation) are the very qualities that can work against them when interacting with Borderlines. Therapeutic conversations that focus on shared experiences are often necessary for establishing trust with BPDs, but they could also reinforce an abuser-victim-rescuer paradigm that becomes reinforced by both participants.
Traumatic bonding (aka trauma or betrayal bond) with people suffering from Borderline Personality Disorder is habitual because they need someone to suffer with them as much as they need someone to care for them. The essence of trauma bonding is loyalty to someone who is destructive (i.e., sacrificing your autonomy and well-being for the sake of accommodating someone’s pathology). Although the therapist may feel like the Borderline’s rescuer and protector, they unwittingly become the enticing and rejecting mother during an “enactment.” Despite the infamous impulsivity of people with BPD, therapists must resist the impulse to coddle away the concerns of their patient via collusion (a countertransference enactment is repetition compulsion of previous relationship cycles with object-other parent representations). If the trauma bond is further entrenched, the therapist will alternate between someone who makes the patient feel secure and someone who makes the patient feel unloved. Basically, the therapist will become the idealized parent for making the patient feel good and devalued as the neglectful parent for making the patient feel bad. This reflexive pattern continues when the therapist is emotionally invested in meeting the demands of the Borderline, especially when the rewards of caregiving outweigh the headaches. Of course, the therapist will never be able to keep up with the pace of appeasement, and they will lose their professional bearings if they try due to the patient’s object inconstancy. In a bizarre plot twist, the BPD patient will declare victimization after devaluing the therapist’s “substandard” performance by temporarily seizing the role of the judgmental and punitive parent. When this occurs, the Borderline becomes the judge, jury, and executioner of the “inadequate child” who is now represented by the therapist. However, the inadequate child is a projection of the patient’s own feelings of inadequacy. After the therapist has been punished for their betrayal, the BPD patient resumes the role of the abandoned-wounded child in need of a rescuing protector. Confused yet? In this mangled network of role-playing mishegas, the Borderline surreptitiously obtains power over authority, only to end up in the same place before they entered therapy. Cluster B chicanery is truly stranger than fiction.
“Just as the infant cannot distinguish between the temporary absence of her mother and her ‘extinction,’ the borderline often experiences temporary aloneness as perpetual isolation. As a result, the borderline becomes severely depressed over the real or perceived abandonment by significant others and then enraged at the world (or whoever is handy) for depriving her of this basic fulfillment,” states Jerold J. Kreisman, M.D. (excerpt from the book I Hate You—don’t leave me)
Borderlines can be very open about personal information, sometimes to a graphic degree, but therapists must remain dispassionate whenever conversations begin to blur professional boundaries. Do not get caught in the patient’s tsunami of effusions, war stories, or efforts to procure collusion through overidentification and triangulation. Furthermore, avoiding discussions about the limitations of therapy with a Borderline only postpones the inevitability of future disappointment and abandonment rage whenever limitations are necessary. Talk is cheap, but the consequences of misguided communication are not. Borderlines take things personally, literally, and have difficulty understanding figurative speech. They need reassurances that are concrete, but absolute compliance with their expectations is futile. Volunteering to become a clinical marionette at a BPD patient’s disposal is nothing less than professional abnegation that gradually occurs as a consequence of trying to please the unpleasable (it’s common for Borderlines to think of therapy as a form of customer service). It’s better to speak cautiously and carry a big boundary. A Borderline’s gift for cagey misdirection is so formidable that it can overpower a therapist’s skill for redirection, thereby creating a clinical version of the Thucydides Trap. To “defeat the therapist” is how a patient with primitive defense mechanisms will use aggressive interpersonal tactics to avoid the discomfort and shame of surrendering their protective veneer. Therapists who are generally non-confrontational must find ways to engage in measured confrontation when necessary by practicing being assertive and comfortable with their own aggression. However, if the bargaining chip of self-sacrifice is enacted (masochistic surrender), the therapist is headed for an impossible task of perpetual mollification. For analogy’s sake, repeatedly soothing a cancerous outbreak with corticosteroids may temporarily reduce pain and inflammation, but it won’t remove the patient’s tumor. Borderline Personality Disorder is essentially a form of emotional cancer; in some cases, it can metastasize beyond remediation (e.g., delayed diagnosis with poor prognosis in older patients). The compulsion to appease a patient with BPD may also occur if the therapist is reminded of urgent demands imposed upon them by their own family of origin (i.e., having a disordered parent). In these cases, the therapist is subconsciously trying to reason with, soothe, and repair what could not be remediated in their past. However, Borderlines identify with suffering because being in pain or creating drama was often the only way they received nurturing from a caregiver during childhood. Although BPDs may plead with others to resolve their suffering, they’re ultimately too afraid to let go of what they know best. Ironically, attempts to remove a Borderline’s agony through reparations only provides more attention to their suffering, which reinforces learned helplessness. In other words, the subconscious motivation of a person with BPD is to continue suffering rather than working to coordinate a successful relief program. Borderlines are not looking to “get better” as much as they’re looking to feel better by locating a sponsor to vindicate and assuage their pain. The most terrifying prospect for a Borderline is to take away their emotional dependency through exposure, because maintaining dependency minimizes separation insecurity. BPDs want to be saved from themselves, but yet they resent being rescued because they feel at home with their maladaptive version of self-determination due to their fear of engulfment. Likewise, people with this disorder tend to make decisions on impulse or delay decisions indefinitely out of fear. Nonetheless, Borderlines will unconsciously use therapists to fulfill object-other roles that were denied in childhood (i.e., the all-loving parent) or fantasies unattainable in adulthood (i.e., the all-giving partner). Likewise, therapists may capitulate for purposes of correcting former attachments gone awry in their own life, or to receive affirmations of caretaking competency. The chemistry of familiarity is a toxic brew, and it all starts with a conversation.
Lookin’ for love in too many faces. — Johnny Lee
Transference by the Borderline and countertransference reactions by the therapist will inescapably emerge as sessions progress. Countertransference occurs with all mental health patients, but it’s particularly problematic with BPD patients. Masterson (1990) views countertransference as a prominent issue with borderline patients because the phenomenon “combines the intensity of the patient’s transference acted-out projections, and the human vulnerability of a therapist.” Additional therapist-patient transference problems may occur because of age, shared interests, family of origin similarities, historical commonalities, and other forms of connection that may result in overidentification. Furthermore, Borderline patients often engage in mirroring, which creates the illusion that they are “the same kind of person” as their therapist. In such circumstances, the therapist may feel like they’re interacting with a version of themselves, or someone who is unusually familiar and accessible. The reality is that the BPD patient is acknowledging or imitating some of the therapist’s most obvious characteristics to attenuate their own anxiety while attempting to facilitate acceptance. In the process, the therapist will naturally respond in a positive manner and the patient with BPD will hold on to that response as a way of creating a safe internalized representation (i.e., “the all-good therapist”). Because Borderlines lack whole object relations, they’re stumbling around to see what you’re made of. As a result, they get some things right, some things wrong, and many things incorrect for purposes of forming their idealization fantasy. The therapist is basically being essentialized, objectified, and instrumentalized, even though it may feel like the patient is doing this for non-pathological reasons. By copying the therapist’s behavior (mirroring), or by agreeing with his or her values, the Borderline patient obtains a false sense of security. Subsequently, therapists may get caught up in the flattering effects of being emulated. However, BPDs don’t want idealized others to deviate from their tenuous caricatures or perfect images, because change equals unpredictability. As a result, their essentialized version is profoundly unrealistic and capable of deteriorating when least expected. Whenever you start to move away from this absurdly unsustainable characterization, the Borderline patient will panic and typically respond with anger and devaluation. Borderlines have no idea who you are, because they have no idea who they are. A BPD’s fear of abandonment means they also fear the abandonment of their internal representations (introjects). Similarly, the therapist may automatically internalize the patient’s false self and become shocked when the Borderline deviates from this gloriously constructed image.
Remember, the intimate nature of therapy is magnified whenever working with Borderline patients because of their intense need for attachment, which creates an infectious intensity. Borderlines like to be liked, and therapists like to be appreciated by their patients. However, communicating with BPDs is a bewildering lesson in psychological hermeneutics, and understanding what’s really being communicated requires careful analysis. For example, idealization of the clinician is a splitting phenomenon with BPD patients who become overly enamored with anyone who is in a position of caregiving (adverse idealization transference), and this may include excessive courtship behavior known as “love bombing.” Idealization is both a defense mechanism and a way to acquire positive mirroring from a parental figure, but it’s also a form of misrepresentation. In addition, the manifestation of idealization could include everything from the clinician being “better” than the patient’s former therapist to being “the best therapist ever.” Compliments can range from reasonable to outrageous, but the emotional conviction of the BPD patient is sincere during those moments. Borderlines are very good at making others feel good so that they can feel good about themselves, and their emotional intensity adds sizzle to the praise. Being zapped by the stun gun of idealization may prevent therapists from seeing who their patient really is, or what they’re capable of after the compliments fade. When a therapist is immobilized by encomiums, the Borderline patient is often seen as innocuous, alluring, or endearing. Not surprisingly, most therapists enjoy being admired for their efforts to provide support, comfort, advice, and reassurance, regardless of the patient’s tendentious proclamations. After all, therapists are human beings who have their own needs for validation in an otherwise thankless, stressful, and emotionally grueling profession. Nonetheless, this “admiration” often comes with a trapdoor that includes eroticized transference (an intense, vivid, irrational erotic preoccupation with the therapist characterized by overt, seemingly ego-syntonic demands for love or sexual fulfillment that goes beyond normally expected expressions of erotic transference). This transference dynamic can intensify because the therapist is literally being paid to pay attention to their patient through empathic attunement and unconditional positive regard. Idealization will make a therapist feel valued, but it has no intrinsic value (aka “cocaine for caregivers”). If, for example, the therapist misinterprets the Borderline’s idealization for genuine appreciation, a chain of events could result in the patient’s desire to establish a corrective relationship. In such cases, the therapist may feel simultaneously drawn to the patient’s desperate need for connection and express malignant eroticized countertransference, especially if the therapist is unable to displace or sublimate their own feelings (a Borderline’s attachment style can activate mirror neurons and release bonding hormones, such as oxytocin and vasopressin). Borderlines often boost the self-esteem of their closest supporter in hopes that their supporter will return the favor, because self-esteem is a rare commodity in the Cluster B warehouse of reverberating deprivation. Likewise, fantasies of “making up” for the patient’s dismal past might occur, especially if the therapist’s positive countertransference is not monitored with sufficient reality testing. The idea of helping the “helpless” is seductive because it induces caregiver’s grandiosity (the Healing or Savior Complex). In this sense, the patient’s idealization of the therapist may result in reciprocal idealization of the patient, which often appears via favorable documentation.
As therapeutic dialogue resumes, the Borderline’s intense need for attachment may become increasingly problematic for therapists who fail to identify or manage positive countertransference reactions (the pulling power of this pathology can be exceptionally difficult to resist once co-idealization has been solidified). Idealization transference is a clandestine invitation to establish an uninterrupted symbiotic connection (“If you are good, I am good”) and it begins as a unilateral decision in the mind of the Borderline; however, idealization should be interpreted as a cry for help rather than an amorous overture. As the Borderline patient attempts to mirror their therapist, the therapist may become a mirror that reflects the Borderline’s inflated self-image by unwittingly encouraging their false self. Nonetheless, for people with BPD, caring is often conflated with physical demonstrations of caregiving, even if their pronounced sensuality and neediness is infused with apprehension and abandonment rage. After all, if nobody else can love the Borderline as they are, at least they can count on their therapist for the type of unreserved acceptance normally reserved for a parent-child relationship, right? Incorporating a healthy paternalizing transference can be useful initially to get the patient to commit to a stable course of treatment, but it must not extend beyond that juncture. History shows that the human intellect is no match for the power of eros. It turns out that Freud was right after all.
The patient is not satisfied with regarding the analyst in the light of reality as a helper….the patient sees in him the return, the reincarnation, of some important figure out of his childhood or past, and consequently transfers on to him feelings and reactions which undoubtedly applied to this prototype….This transference is ambivalent: it comprises positive as well as negative attitudes towards the analyst, who as a rule is put in the place of one or other of the patient’s parents, his father or mother. — Sigmund Freud
“Because of the centrality of projective identification in the experience of treating borderline patients, therapists often feel invaded and transformed into someone other than who they are. Attempting to resist this transformative process can be a formidable problem. Firm boundaries and reasonable limits will eventually reduce the patient’s infantile demands. When the therapist refuses to be the idealized, perfect parent, patients will ultimately learn that they must become their own mothers—the wish to fuse and be fed must be turned inward,” says Dr. Glen Gabbard.
As James F. Masterson (1976) noted, “Probably the single most difficult skill to acquire in psychotherapy of borderline patients is the ability to recognize and control one’s own identification with their projections.”
From an article in the Clinical Social Work Journal entitled The trainee and the borderline client: countertransference pitfalls: “Countertransference will be broadly defined as distorted thoughts, feelings, and attitudes toward the client, either consciously or unconsciously held. For the borderline patient, the definition should be expanded to state that the countertransference is a response to the transference inspired behavior of the client. Borderline transference will be defined as a manifestation of the borderline psychopathology, which involves relating to the therapist as a tantalizing omnipotent, but potentially abandoning, parental stereotype. It is based on primitive object representations that are largely unavailable to the therapist. The transference contains magical expectations of infantile wish fulfillment that, if unwittingly encouraged, cause numerous problems for the therapist.”
According to the Encyclopedia of Psychotherapy: “Activated countertransference carries the burden and seduction of a compulsion to take action. Intense admiration, idealization, erotic feelings, and rescue fantasies for the patient seem so compelling that the impulse to action is irresistible for some. These reactions become problematic when the therapist loses his or her sense of control of the therapeutic relationship and begins to feel that he or she is there for a different reason, such as to rectify a wrong in the patient’s life or to provide comfort when insight is more appropriate.”
Rule of thumb: Never go full transference gratification. The key to avoiding countertransference pitfalls is to recognize when countertransference is occurring. Getting lost in the drama of countertransference enactments usually happens when therapists lose themselves during the process of pacifying their patient. To become a Borderline’s “favorite person” is to become a stabilizer of a morbidly unsustainable proposition. Enabling by accident can result in some very serious accidents.
We’re far from the shallows now. — Lady Gaga
Borderlines can pressure therapists into becoming psychosocial saviors if their purported tales of victimization and historical discrepancies are not thoroughly investigated. Fear and denial keep people with BPD from doing any emotional heavy lifting, so they become experts at deflection and projection by reorganizing factual accounts to avoid personal responsibility and feelings of shame (experiential avoidance). As a result, therapists might feel responsible for doing more than they should if they’re swept away by the patient’s anecdotes of adversity. Therapists are trained to be of service to those in need, and Borderlines survive by getting others to serve them. Unfortunately, much more will be expected than the therapist can provide because of the patient’s lack of object constancy and inability to self-soothe in a healthy way. It could be argued that object/introject inconstancy represents the core of this disorder (an inability to maintain a stable emotional bond with an intimate other or a stable sense of self and others). Consequently, perceptions of others are unrealistic, fluctuating, and fleeting. A Borderline’s identity diffusion and fear of abandonment are likely epiphenomena caused by the undeveloped mechanism of alterity (separation-individuation) that allows for object constancy. This would also explain the incessant trust issues endemic to this personality disorder, including James Grotstein’s “black hole” metaphor when it comes to the futility of pacification by concerned others. Insufficient maternal bonding during infancy is a sufficient factor for incurring this deficiency, but additional trauma during early childhood only makes the problem worse. If this premise is correct, it would explain why a person with BPD has poor psychosocial proprioception. Everything is ridiculously ephemeral, and nothing is ever safe enough, good enough, reassuring enough, or caring enough. Meaningful change that requires flexibility is intolerable because it’s a simulacrum of object inconstancy, hence active-passivity, which renders other people useful or disappointing. In fact, other people are as perceptually inconsistent to the Borderline as their emotions and moods, thus resulting in fear, paranoia, and all the must-see TV drama that follows. How can something (self or others) be trusted when it never seems dependable? If you can’t trust your inner experiences, how can you trust the world around you? The world is forever pivoting on the BPD’s lack of object constancy, and everything needed to be reliable is evaporating (abandonment) faster than its ability to provide stability and reassurance. When faced with such an unusual deficit of interrelatedness, the therapist could end up responding like everyone else in the Borderline’s life—attending to the never-ending needs of a desperate castaway in search of a supportive audience. If this occurs, the therapist will be baptized as the patient’s object-constancy generator, which may push the therapist into deeper waters. Unfortunately, providing reassurance beyond a clinical context puts therapists at professional risk. In fact, the Borderline’s desire for constant contact is one of the biggest causes for crazy making because it’s both confusing and unappeasable. The patient’s lack of object constancy will induce strong feelings of responsibility and indispensability in their therapist. Subsequently, the patient may feel entitled to rely on the therapist for object constancy because they’re the only person who seems committed to providing validation and safety. However, the more a therapist tries to address this developmental deficit by becoming a human harbor and loyal taskmaster, the more conspicuous the patient’s object inconstancy becomes, thereby creating a tar-baby dilemma. As a result, the therapist may unknowingly represent the most recent rescuer in heavy rotation on the Borderline’s take-care-of-me carousel.
“Borderline patients are notorious for evoking deviations from the therapeutic frame that lead to ill-advised boundary crossing. These patients may feel a specific form of entitlement resulting in demands to be treated as exceptions to the usual procedures,” according to Dr. Glen Gabbard.
From the American Addiction Centers: “People with BPD have relationship issues with nearly everyone in their lives, and significant relationship issues will often develop with therapists as a result of the therapeutic process of change. The patient may first idolize the therapist and then later totally demonized them (splitting) or may attempt to manipulate different therapists against each other in order to manipulate the overall treatment. Professionals who treat people diagnosed with BPD must be aware of these potentialities and even expect them to occur. Unstable personal relationships within treatment itself as well as outside treatment contribute to the difficulty of helping these individuals adjust.” However, the limited time frame of therapy is not equipped to withstand such relentless permutations of interpersonal stratagem. As a consequence, the therapist may begin entertaining taboo thoughts of attending to the patient’s psychosocial “emergencies” outside of a clinical context. Without maintaining boundaries, the therapist will no longer be able to maintain objectivity; without maintaining objectivity, the therapist will forever be trying to extinguish the patient’s peripheral complaints instead of addressing their core issues. Borderlines unconsciously manufacture their own misery, but they can make anyone who attempts to alleviate their misery feel equally miserable. Like a swift-water first responder, the therapist will drift farther and farther down the gauntlet of BPD appeasement until the rescue raft of good intentions finally capsizes. The helping profession of psychotherapy encourages the development of a strong relationship to help the client, but it’s the professional aspect of the relationship that must be prioritized whenever working with Borderlines. In the BPD motorcade, the wheels of impulsivity are always out of brake fluid—it’s like having a hyperactive limbic system for an engine without access to a steering mechanism. If the therapist mistakenly hands over the car keys, the Borderline patient will drive everyone off the nearest cliff with their busload of needs. Meanwhile, the therapist should prepare to be thrown under the bus whenever those needs are no longer being gratified (people with this disorder fail to realize that throwing someone under the bus does not make them a better bus driver). It’s the parable of the scorpion and the frog writ large.
Dr. Thomas Gutheil describes the “you’ve gone this far” rationalization for boundary crossings, in which the patient points out that some boundaries have already been crossed and thus further transgressions are required or demanded: “Therapist guilt about past boundary transgressions may be the driving force behind agreeing to continue. Conversely, threats of complaint about early boundary issues may frighten or coerce the treater into continuing or expanding the crossings.”
Change begets change as much as repetition reinforces repetition. — Bill Drayton
Addressing the continuous demands of a Borderline corresponds with The Myth of Sisyphus; it’s utterly exhausting and operationally futile. There’s not enough coffee in the galaxy to keep up with a Borderline’s level of impulsive energy and supernova of needs. BPD patients will make six impossible demands before breakfast, but any effort to fulfill those demands will result in six more demands before lunch and dinner. Borderlines are mental health patients without patience, so they must win the war of acquisition through attrition. Adrenaline prevents boredom, because boredom breeds dysphoria. The problem is that Borderlines largely identify with the drama of their problems, so any attempt at remediation threatens their victim identity. Lacking in object constancy, there’s never enough words of reassurance or altruistic gestures to placate a BPD’s need for consolation—you might as well be sweeping a dirt road. In such circumstances, the therapist may find themselves making promises equivalent to the demands of the Borderline in an effort to reduce emotional reactivity; attenuate impatience; soothe anxiety; alleviate loneliness, or to continue receiving accolades as an intrepid caretaker. As this temerarious gambit commences, the BPD patient will invariably become more dependent on the therapist’s attempts to stabilize their moods and precarious sense of self. Meanwhile, therapists may become “addicted” to eliciting positive changes in the patient’s emotional state by becoming a crisis caddie, “all good” object, or parental substitute. The Borderline’s coercive ability to reshape their therapist into becoming a more responsive caretaker allows them to maintain centrality in the unfolding psychodrama. Predictably, most therapists will feel professionally authenticated by gestures of admiration—willing to risk more and more for the sake of accommodating their client. Therapists who allow clients to exploit their generosity often have people-pleasing tendencies. In addition, therapy sometimes encourages dependency with clients who lack self-efficacy as a consequence of the power differential—implicit in the medical community is the suggestion that you’ll be taken care of when you’re suffering. It’s easy in these situations for therapists to feel revitalized by offering levels of emotional support, comfort, and advice that are supposedly unavailable to their client in other contexts. After all, if positive psychology teaches us that finding a sense of meaning and engagement is curative, nothing could feel more meaningful for a caregiver than assisting someone who appears helpless and unambiguously appreciative. However, the BPD’s veneration of the therapist is always contingent on a continuation of appeasement within the therapist-patient validation pyramid scheme. No matter how intoxicating reciprocal validation feels during the ascending honeymoon period with a Borderline, the end result will invariably lead to emotional bankruptcy, disappointment, and rage. Although idealization is a potent dopamine generator, therapists should take immediate precautions if they become the subject of pedestalization. Adulation by people with BPD is invariably followed by animosity; the cling comes before the sting. Borderlines and caretakers can become lock-and-key participants in a swamp of creeping codependence, and this indelicate union involves countless caveats that predict the worst possible outcomes for all participants. People with BPD will use their brand of luminol to expose the bleeding hearts of anyone who is willing to be subservient to their emotional needs, but it’s a one-way street without lampposts. Once the lifeblood of caregiving capitulation is located, Borderlines become merger-hungry hemovores of opportunism. Although the term “emotional vampire” is an epithet, the principle of needing others to survive is at the root of emotional dependency.
“Clinicians should be prepared to recognize this effect and then explore with patients whether their hope for such care is realistic and, if so, whether it is good for their long-term welfare. When the decline of functioning is sustained, it may mean that the focus of treatment needs to shift from exploration to other strategies (e.g., behavioral modification, vocational counseling, family education, or limit-setting). Of special significance is that such declines in function are likely to occur when patients with borderline personality disorder have reductions in the intensity or amount of support they receive, such as moving to a less intensive level of care. Clinicians need to be alert to the fact that such regressions may reflect the need to add support or structure temporarily to the treatment by way of easing the transition to less intensive treatment. Regressions may also occur when patients perceive particularly sympathetic, nurturant, or protective inclinations in those who are providing their care. Under these circumstances, clinicians need to clarify that these inclinations do not signify a readiness to take on a parenting role.” — (excerpt from Practice Guidelines for the Treatment of Patients with Borderline Personality Disorder).
I went down, down, down and the flames went higher. — June Carter Cash
The therapist might regrettably believe that professional boundaries aren’t going to be effective in addressing this patient’s needs. In fact, the therapist may have never encountered a patient who is so oblivious to standard rules of engagement in a clinical setting (BPDs were often raised in households without personal boundaries). Lacking in alterity, the separate identity of the therapist is not recognized by a Borderline; it’s idealized, reformulated, and instrumentalized. In fact, the therapist is unknowingly fulfilling regulatory roles based on the needs, fears, and fantasies of the patient. Torn between reluctance and intrigue, the therapist may find themselves drifting into inappropriate territory at the behest of their patient, as if they were being pushed by a cyclone of conflicting emotions and desires. The word inappropriate is commonly used to describe BPD behavior, because Borderlines cannot relate to others in age-appropriate ways. Borderlines encourage regression and discourage differentiation to create a safe space by immobilizing any interaction that provokes separation insecurity. Conversely, therapist must encourage differentiation and discourage regression. If a therapist feels intimidated by the patient’s imperative-driven thinking and infantile demands, a “Borderline Without Borders” situation will eventually consume the therapeutic frame. Additional fears of being perceived as uncaring or inaccessible during therapeutic interactions may cause therapists to feel guilty or inadequate. As a result, exceptions to standards of care are usually made to keep their “special client” engaged (aka VIP syndrome). BPDs occupy a privileged position as mental health patients, because they often respond in treatment according to the whims of an unruly child while being granted the respect and legal rights of an adult. In some situations, therapists may feel as if they’re being negligent by upholding professional standards. Borderlines also have an aptitude for making others feel responsible for their feelings, and the gravity of this burden can turn some caregivers into deferential doormats. Crying spells and irritation during periods of despondency may compel therapists to provide comfort through proximal reassurance. Of course, comforting a Borderline is like trying to diffuse a bomb if you don’t respond within the particularities of their hypersensitive expectations (anything you do or don’t do has the potential to upset them even further). Feeling like an unwanted “monster” when they were growing up can result in behaving like a monster around others who inadvertently trigger their childhood trauma.
The Borderline’s intense psychological pull has the capacity to draw therapists into their kaleidoscopic world of emotional mayhem without realizing the depths of their emptiness. Furthermore, an erroneous belief may emerge that accommodation must dictate the direction of all future interactions without realizing that adequate accommodation is impossible. In other words, the rules of therapist-client engagement become secondary as the therapist is provoked by growing confusion on how to respond to their patient’s needs. In everyday circumstances, it’s advised to avoid or limit contact with those suffering from untreated personality disorders; however, therapists have no other option but to engage with caution or to initiate an appropriate referral if available. Subsequently, some therapists may already be digging their clinical grave sites with a shovel made out of sheer gullibility. To be sure, Borderline patients will defy boundaries without compunction while expecting their therapist to suspend the reigns of professionalism if therapy is perceived to be uncomfortable. BPDs can “play nice,” but only if you’re following their shifting rules and expectations. People with BPD do not trust others because they couldn’t trust their parents; furthermore, they can’t trust themselves. Most importantly, therapists must not let their objectivity become a slave to the Borderline’s subjectivity. For example, if a boundaryless zone is established out of respect for a patient’s level of discomfort, therapists should expect an escalation of efforts to dominate the direction of all subsequent interactions. Whenever the floodgates of unconditional acceptance open up, Borderlines become Dionysian tornadoes bent on annihilating the Apollonian structures of psychotherapy. Patients with BPD can be rewarding to work with if you know what you’re doing, but you must always be aware of the fine print on the Cluster B box of combustibles. The only predictable variable when working with this population is unpredictability.
“This good and bad dichotomy plays out in the therapist’s office. The client may try to entice the therapist to gratify their dependency needs and the therapist may feel compelled to collude with the client’s regression. If the therapist does not gratify, but rather confronts the lack of responsibility, for example, then the client may feel abandoned and compensate with rage, seeing the therapist as ‘mean’ and not supportive. Therapists unconsciously collude by giving too much advice, not expecting the client to act responsibly in all situations, and tolerating acting-out behaviors. The therapist may fear the client will judge them harshly and leave if they are too confrontational,” states Dr. Patricia Frisch.
Classification of erotomania has always been object of debate. J. Reid Meloy formulated the hypothesis that there are two forms of erotomania: One traditional form, clinically accepted as delusional erotomania; and another “borderline” type in which there is no clear delusional disorder but rather where there is a major attachment or binding pathology colored by symptoms of continual pursuit and potential violence towards the erotomanic object. This second form of erotomania is characterized by its narcissistic, hysterical, paranoiac, and psychopathic traits. The degree of the disorder is determined by the discrepancy between the object’s emotional attachment to the erotomanic and the intensity of the erotomanic’s attachment to the object. For this type of erotomanic, relational intrusion is persistent and separation from their target is perceived as rejection and humiliation. This perception awakens rage-like feelings of abandonment that could result in chronic harassment, stalking, or death (aka Fatal Attraction Syndrome). The unexpected emergence of erotomania in a treatment setting can become extremely dangerous to the professional integrity and well-being of the therapist while developing a therapeutic alliance. Stalking is a pathology of attachment (Meloy, 1992), often driven by the force of fantasy (Person, 1995). In particular, erotomanic stalking is not amenable to reason and does not respond well to normal methods of deterrence (legal or otherwise). In the end, stalking is about power and control (emotional terrorism towards their target). Unfortunately, patients can become love obsessed with their mental health provider due to the intimacy of therapeutic communication and the nature of therapeutic alliances. Clients who stalked therapists fell into three broad categories: those clients who were needy and made early attachments to their therapists; those experiencing erotic transference; and those with personality disorders. According to Meloy, “Stalking motivated primarily by a personality disorder and fueled by abandonment rage will generally show a poor response to mental health interventions, especially if the subject is antisocial or worse, psychopathic. In the latter case, treatment should not be considered, since there is none, and aggressive prosecution is recommended to ensure lengthy segregation from their target. Most habitual criminals and obsessional followers are pathologically narcissistic and their intolerance of shame, defensive rage reactions, inability to grieve loss, and compensatory fantasies of entitlement and retaliation should not be forgotten. The abandonment rage fuels the subject’s pursuit, with an intent to devalue the object in real life, paradoxically restoring the subject’s narcissistic linking fantasy to the idealized object.” *Borderline patients do not need an additional diagnosis of erotomania to engage in stalking behavior.
For the erotomanic, negative attention is better than no attention at all. It’s their psychotic melodrama, and your participation is not needed to perpetuate the obsession. Nonetheless, you’re at the mercy of an obsessive, paranoid, and possessive mind. Risk assessment must precede client engagement because fixation becomes the erotomanic’s substitute for healthy human connection. Some delusional convictions can be as compelling to therapists as they are to the client, especially if these beliefs are presented as minimally counterintuitive propositions. Delusions are categorized by the nature of their content, such as persecutory, grandiose, somatic, and erotomanic delusions or delusions of jealousy or reference. If erotomanic delusions are misinterpreted, the therapist may confuse the client’s attachment-driven psychosis with an intense connection that transcends the therapeutic framework. Aspects of the therapeutic relationship can produce misunderstandings about the nature of the intimacy generated and about appropriate boundaries. Empathy or assistance from an authority figure may be interpreted by the erotomanic as evidence of true love. Consequently, the therapist may feel overwhelmed or aroused by the prospects of attending to such erotically charged inducements (i.e., falling in love with the idea of making the client feel loved). As a result, two people become entangled with the power of a delusion. Reality testing breaks down and the distinction between patient and therapist becomes obsolete. It’s a textbook example of folie à deux.
What the erotomanic desires, experts say, is an idealized romance that resembles a spiritual union. As noted in the book I Know You Really Love Me by Doreen Orion, M.D., “An abiding problem with managing these cases is the almost total lack of motivation for treatment. Those caught up in pathological love do not see themselves as ill, but as blessed with a romance whose only blemish is the tardiness of response in the beloved or the interference of third parties (often including the would-be therapist). The benefits of these disorders for the patient should not be forgotten, for they provide some solace for their loneliness, some support for their damaged self-esteem, and some purpose to their otherwise empty existence.”
“The object of affection becomes an ink blot, a Rohrshach test,” says Stuart Fischoff, professor of psychology at California State University, Los Angeles. “Whatever the object of desire says, the delusional lover brings into it anything he or she wants.” In other words, it’s the erotomanic’s movie and your part is not fully revealed until the credits start rolling. Because erotomanics have an egocentric bias, they’re perpetually attributing unrelated information as personal messages from their object of attachment. Not being in contact can be as problematic as occasional contact, because the search for signals (both positive and negative) keeps the erotomanic from feeling disconnected. The pathological process of delusional misinterpretation of perceived signals from the social environment itself may result from poor reality testing due to a failure of social meta‐cognition. In clinical training, therapists learn to put their patient’s welfare before their own, which makes it easy for them to underestimate or deny the potential for danger in certain situations. If the therapist hasn’t been burned alive by the BPD house fire, they may get chewed up in the erotomanic meat grinder. “A lot of the times, people can go on with their life, ostensibly normally and not have any perceived psychotic disorder,” says Meloy, who has stumbled across erotomanic behavior in his patients while treating them for other conditions. “It surprises you. You don’t know that it’s there.”
Characteristic of erotomanics is la belle indifference, which explains how they can profess to love their victims and yet remain so indifferent to the pain they cause them (Zona, Palearea, & Lane, 1998). An erotomanic almost always displays la belle indifference toward the suffering of their victim, and the complete disruption in the victim’s life they have caused. In this way, erotomanics are narcissistic in the true sense of the term; only the suffering they have experienced at the hands of their capricious “lovers” counts, because they believe, with all the unshakeable conviction of delusional truth, that they are entitled to a relationship at any and all costs to their victims (Orion, 1997).
Yeah, yeah, my shit’s fucked up; it has to happen to the best of us. — Warren Zevon
A veritable recipe for disaster awaits therapists who are coping with issues of their own, such as compassion fatigue, major life transitions, marital issues, family problems, work stress, anxiety, or depression. To be certain, there will come a time in every therapist’s career when their personal problems might match or surpass those of their patients. Improving the lives of others leaves little time for improving one’s own life, and treating an untreated Borderline is an insurmountable challenge if the therapist is not operating on all cylinders. Therapists must suppress their emotions due to the nature of their work, but this occupational necessity can make working with BPDs exponentially problematic. Contrary to professional stereotypes, therapists are not emotionally impervious automatons, and many come into the field with their own trauma history (wounded healers). Furthermore, working with trauma can be like working with asbestos, and reactivation of trauma occurs through exposure. Therapists, by definition, are expected to be accepting, non-judgmental, calm, and supportive of their clients, but the process of therapy can be emotionally draining because clinicians are constantly shifting gears to meet new challenges. Because people with BPD experience the world through a labyrinth of dysregulated emotions, the therapist must work even harder to manage theirs. As a reminder, a therapist’s unresolved conflicts, family history, stressors, and personal problems often become magnified through transference-induced provocations whenever interacting with mental health clients, but especially when conducting therapy with Borderlines. A reliable axis of balance is required in the therapist’s life before being able to identify various degrees of imbalance in others. Likewise, losing one’s proverbial mind can sometimes occur as a byproduct of treating those who have already “lost” theirs (e.g., vicarious traumatization, compassion fatigue, and burnout). Overall, working in mental health can be detrimental to a clinician’s mental health. Therapists do not have all of the answers, but they’re often expected to provide quick solutions and immediate relief for patients who do not understand that therapy is a process beset by uncontrollable variables, inconsistent treatment responses, and diagnostic dead ends. Borderline patients, in particular, can overwhelm therapists with their impatience and inconsolability. However, if therapists acquiesce to avoid conflict, therapy will eventually become a meeting of the minds with two minds short. The effects of unresolved trauma and vicarious traumatization can also result in therapists trying to heal themselves by healing their patients. When working with trauma-related psychopathology, desires to “repair” the patient may represent an unconscious motivation by the therapist to address their own issues. Additional problems occur when a therapist in crisis begins to rely on emotional support from their patients (a therapist in crisis cannot adequately help others in crisis). Therapists must not allow social work to become their social life, or else they’ll start to blend in with their patients. Burnout is gradual, and therapists are usually unaware of its insidious effects. Elements that may cause burnout include a lack of control, unclear job expectations, dysfunctional dynamics, oppressive workplace, monotonous tasks, chaotic work environment, high workload, and work-life imbalance. Therapists need therapists too. Without proper self-care, the ability to provide the best care for their patients will eventually disintegrate. Errors of judgment happen more frequently when therapists are at their wit’s end (chronic psychosocial stress reduces neuronal activity in the dorsomedial prefrontal cortex), and therapists who continually give too much of themselves are more prone to burnout. Because the onus for countertransference misadventures is always the responsibility of the therapist, being fit for duty matters. There is no stress greater than the stress of trying to absorb the miseries of the world. Being a human repository for other people’s frustrations, unhappiness, horror stories, fear, loneliness, shame, and anger can make therapy a very stressful, emotionally challenging, and sometimes dangerous occupation.
Well-Functioning is defined as the enduring quality in the therapist’s professional functioning over time, and in the face of professional and personal stressors (Coster & Scwebel, 1997). Therapists have many factors to contend with in life and practice aside from the dynamics of working with borderline patients. The most common personal problems interfering with therapist well-functioning are emotional exhaustion and fatigue (Mahoney, 1997).
For the clinician, it may be just another day at the office; but for the Borderline, it’s survival of the neediest. This is why ongoing supervision and consultation are essential, including a willingness by therapists to accept objective input and monitoring. Therapists shouldn’t be afraid to ask for help when they’re in doubt (there are infinite reasons why continuing education is important). In fast-paced clinical settings, there may be insufficient bandwidth for pursuing in-depth analyses of complicated psychiatric patients. Ongoing administrative tasks, demanding clients, and continuous emergencies can condition therapists to become perfunctory multitaskers, adrenaline junkies, and trigger-happy fire extinguishers. Of course, no client is better at building fires than a Borderline. The emotional exhaustion of caregiving is difficult enough without having to manage an emotionally unstable client. When it comes to the business of mental healthcare, the phone is always ringing with bad news. Therapists often feel frustrated by their inability to do more for certain patients, and Borderlines invariably provoke additional feelings of incompetence. Challenging a thin-skinned person with BPD is much more difficult when the therapist is already worn thin from various occupational stressors. BPDs can expose a therapist’s deepest insecurities while causing them to question their clinical expertise. Borderlines will figure out the combination lock of amenability to avoid rejection and latch onto the therapist’s willingness to act as an external regulator with uncompromising vigor. Without proper training for early identification and comprehensive management of BPD, therapists are potentially lost in an ocean of misapprehensions and clinical missteps. Working with a misdiagnosed Borderline is like conducting therapy in Plato’s Cave, because the client’s fractured identity will present itself as an ongoing mystery—it’s like trying to nail jelly to a wall. If the therapist is not careful, the BPD’s regressive behavior will quickly capture the limelight (there’s always a Russian roulette component to working with high-risk patients).
Logic is an enemy of the emotionally impaired, so don’t fall for the belief that logical arguments or psychoeducation will overcome emotional reasoning. Furthermore, CBT is an insufficient intervention when patients suffer from cognitive deficits and cognitive distortions. However, if you don’t maintain a rational and measured position, you’ll set yourself up for the Borderline’s emotional ambush and the thumb-cuff qualities of projective identification. Consequently, the therapist may become a reluctant participant or a willing accomplice in the BPD’s quest for regressive enmeshment. Soon thereafter, a disconcerting array of rationalizations are incorporated by the therapist to maintain denial about their growing sense of fear, obligation, and guilt (FOG). Other reactions may include pity, excitement, anxiety, and fascination. Overall, it’s the fear of how a BPD will react that keeps clinicians locked into a holding pattern of approach-avoidance that mimics the patient’s interpersonal style of approach-avoidance. Therapists spend their days trying to transform the lives of their clients, but Borderlines have a talent for transforming therapists. With BPDs, the Rogerian maxim should be carefully reconsidered with a strong dose of the conditional.
“The limit of the therapist’s caring is often tested through pushing the agreed parameters and boundaries of the patient-therapist relationship. Prolonged engagement with a nurturing therapist can intensify dependency wishes and lead to desperate attempts to engage the therapist when uncontrolled neediness is triggered. The empathic therapist will detect the patient’s desperation and childlike qualities, and naturally respond with rescue fantasies of his/her own. If treatment parameters are not maintained, a vicious cycle may ensue entailing progressive regression to a helpless, infantile, and dependent state, alternating with rage and/or self-destructive behaviors. The therapist has the feeling that he/she is in the midst of a feeding frenzy,” warns Robert J. Gregory, M.D.
And you may ask yourself, am I right? Am I wrong? And you may say to yourself, ‘My God! What have I done?’ — David Byrne
Pervasive patterns of acting out conveniently thwart BPDs from exploring the origins of their neuroticism. As a result, they never learn to effectively cope with deep emotional wounds. Although dissociation obviates emotional pain, it ultimately prevents introspection and results in more sensation-seeking behaviors. Borderlines, if they are anything, are invariably misunderstood by others. Similarly, they abhor personal criticism and do not appreciate humor at their expense (everything is personal). BPDs believe that other people must acknowledge their persistent feelings of emptiness and emotional suffering. It’s about their feelings, not yours. Borderlines understand the value of the squeaky wheel, but they’ve forgotten the parable of crying wolf. BPDs are not looking for solution-based therapy as much as they’re looking for reassurance, validation, and collusion. Therapy with some clients is like trying to teach someone how to walk again, but Borderlines will become obsessed with the crutches. In addition, BPDs rely on others for advice that is seldom integrated in any meaningful sense (solution implementation is a problem for Borderlines due to active passivity). Assuming responsibility for choices and behavior creates overwhelming stress and anxiety for people with this disorder, because culpability has the potential to magnify human imperfections that provoke shame. Without any diminution in relation to special pleading, the Borderline becomes the insufferable sufferer. A therapist’s decision to suspend protocol for purposes of alleviating a BPD’s unabated separation anxiety, restricted self-efficacy, and recurring pathos is just around the corner if what’s being communicated vis-à-vis is not understood for its deeper implications.
“The ongoing temptation in the psychotherapy of borderline patients is to try to provide gratification for longings that cannot possibly be satisfied in a professional relationship. Indulging the patient’s wishes is a strategy bound to fail and also bound to engender regression by reinforcing infantile expectations, which will only intensify the patient’s eventual rage,” states Dr. Glen Gabbard.
Despite their age, Borderlines must be approached with adequate caution and consistent restrictions. Because of their emotional instability and immaturity, propitiation is a mug’s game. BPDs prefer to outsource causation for their behavior because it prevents the pain of self-reflection. There is no such thing as contingency planning, mindfulness, or comprehensive critical thinking for a mind overwhelmed by emotions. The biggest mistake a therapist can make with a Borderline is to interact with them as if they were rational adults with an age-appropriate sense of personal responsibility. No therapist wants to infantilize an adult patient, but some BPDs require Romper Room referees more than collaborators. As a defensive response, some therapists may become aloof or hostile (negative countertransference) to compensate for the Borderline’s unreasonableness and periodic temper tantrums. However, being too reserved or defensive could lead to accusations of being distant, cold, uncaring, cruel, or judgmental. Caught between the binary position of not caring enough (overemphasizing boundaries) or caring too much (removing boundaries) leaves little room for making “mistakes” in communication, let alone being able to challenge the patient. This oleaginous tightrope is even more hazardous if the therapist is unaware that such boundary testing maneuvers are part of the BPD’s need for unambiguous acceptance. What initially felt like a once-in-a-lifetime clinical opportunity to help someone in need could result in occupational suicide if accidentally mishandled.
But then you let me down, when I look around; baby, you just can’t be found. — Madonna
Borderlines often seek support from those with limited availability because they anticipate abandonment in advance. Of course, whenever this doomed attachment is disrupted, their object of adoration will quickly become an object of aversion. Borderlines view separation as betrayal, and perceived rejection by a caregiver will provoke abandonment rage. Without the availability of a compliant object for emotional support, the former idealization of the therapist quickly evaporates as the BPD’s fear of abandonment begins to surface. Borderlines will search for malicious intent where none exists, and their primary mode of communicating disappointment is through reactionary rage. Without being able to regulate their conflicting emotions, and without being able to make sense of others as separate individuals (lacking in whole object relations), vilification via polarization ensues. Sadly, the therapist has been conditioned by the warm glow of being considered an ideal caregiver and will be confused when “the turn” appears. The emotionally starved and competitive Borderline wants love to be a possession, whereas the therapist may become lovesick in their pursuit of trying to heal their patient. BPD relationships alternate between gluttony and starvation; it’s all or nothing. Ironically, assisting Borderline clients can initially feel invigorating for therapists—the rest of the world disappears as the caregiving lens focuses on rescuing the needy. However, the therapeutic lifeboat will invariably hit an iceberg of Borderline indignation before the clinician finally comes to their senses. People with BPD prefer continuous streams of validation instead of being challenged, and they’re remarkably proficient in achieving such ends. Any ambiguity in the Borderline’s search for acceptance is terrifying, and the prospect of change is unbearable. Borderlines seek stability, reassurance, approval, safety, and unambiguous gestures of affection, but it ends up being at the expense of significant others, family members, friends, and primary caregivers.
I am because my little dog knows me. — Gertrude Stein
I am because my little dog won’t leave me. — Borderline
According to Dr. Robert J. Gregory, “Persons with BPD have been noted to have a need for certainty and for complete understanding from others (Bateman, 1996; Shapiro, 1992). They employ a binary system of logic and attribution that excludes alternative perspectives that may create ambiguity. For example, they may tell their therapists, ‘If you really cared about me, then you would let me call more often. All you care about is your money.’ On the surface, the proposition appears logical and irrefutable. However, there is an underlying assumption that the therapist’s primary mission should be to care and nurture their patients like a mother. There is also an implied dichotomy or split in the perspective of the therapist as either totally caring and accommodative, or totally cold and callous. There is no room in such a polarized attribution system for a more ambiguous and realistic perspective of the therapist as having complex motivations, including some genuine caring for the patient, but within certain limits. What makes working with this population so difficult is the patient’s ability to provoke others into responding in a way that is consistent with the patient’s attributions and expectations. In other words, the patient expects others to behave in a certain way, and the therapist may feel compelled to behave in a way that is consistent with the patient’s expectations—an interpersonal process that has been called enactment. The confluence between the patient’s expectations of others and the actual behavior of the therapist results in reinforcing the patient’s expectations and the distorted attributions of self and other upon which those expectations are based. Therapists may have a difficult time discerning whether negative encounters with a patient resulted from the patient’s attributions and responses or from the therapist’s responses.”
Dr. Perry D. Hoffman, president and co-founder of the National Education Alliance for Borderline Personality Disorder, explained one of the defining aspects of the disorder: “It occurs in the context of relationships. Unlike other psychiatric diagnoses, if you put someone with schizophrenia on an island all by themselves, their mental illness would still be evident. If you put someone with BPD on an island, you wouldn’t necessarily see the symptoms—whatever happens, happens in the context of [interacting] with someone else.”
Instead of becoming a storm chaser, it’s better for therapists to understand the nature of the storm.
I’ve waited hours for this; I’ve made myself so sick. — Robert Smith
Because Borderline Personality Disorder is essentially a developmental and attachment disorder, the client’s neediness and search for parental nurturing is often insurmountable. Overall, BPD is a mental disability that relies on unrealistic accommodation from others for safety, regulation, and reassurance. However, overly attentive responses to the accumulating demands of BPDs will result in an unavoidable crash landing. The problem is that therapists have been issued the caregiving equivalent of a pilot’s license and will be held accountable for any loss in therapeutic altitude. To be sure, many support planes have disappeared while flying solo over the Borderline Triangle. However, if BPD patients could rewind the flight recorder, and muster a modicum of objectivity, they would find themselves bombarding the analytic cabin space and taking over the control panel (people with BPD must learn how to observe and describe their own behavior). Just as the therapist has misinterpreted the patient’s tales of victimhood, the BPD will undoubtedly misinterpret the therapist’s efforts towards appeasement and feel betrayed if extraordinary caretaking promises aren’t kept. This potentially high-conflict personality can become extremely volatile if their chosen protector appears to have forsaken them on purpose. After all, the therapist has been providing a steady supply of validation, reassurance, and emotional support in a safe holding environment, which unintentionally turned the therapist’s office into the BPD’s pathological supply space. Unprepared therapists will be marinating in a clawfoot tub of Cluster B bathwater before waking up to find themselves circling the drain. Emotional riptides in the Sea of BPD can quickly sweep therapists into shark-infested waters. If the Borderline’s sense of identity is experienced as being dependent upon a stabilizing other, the therapist has just abrogated the client’s recognition of self—it’s like denying refills on life-saving medication. Treatment of this disorder depends upon the availability and compassion of others, but this disorder is also perpetuated by the availability and compassion of others. The therapist has unwittingly been serving as the BPD’s missing internal parts, and now those parts are wearing out (destabilizing the stabilizer). In the end, Borderlines will pull the rug of congeniality from underneath their caregivers whenever the support cart goes off the rails (cessation trauma). The Borderline’s dichotomy of self will vacillate as the previously dependent victim becomes the omnipotent avenger. With record-breaking speed, the former idealization of the therapist is replaced by a 180-degree devaluation phase. A critical threshold of stress has been reached and the “Borderlion” within has been unleashed. Negotiation is pointless—it’s like trying to simultaneously de-escalate and outrun a cheetah. Uncomfortable feelings are not permissible, and the most negative and paranoid interpretation of events will be the BPD’s final interpretation. No catastrophe left behind. What was once an entirely “good” object is now a completely “bad” object (splitting), because there is no middle ground in the Borderline’s world of internalized object-representation. An overwhelming desire to feel safe again compels BPDs to bifurcate people, messages, and situations into digestible categories.
Borderlines consistently put their needs at the forefront, so any sudden reduction in attentiveness will always end badly. If the therapist acquiesced to meet the needs of the Borderline until now, there must have been an ulterior motive (they might even make bold assertions about the “sinister motivations” of the therapist). In fact, most BPDs don’t know how to interpret generosity or compassion because of the contingent “love” offered by their parents (i.e., rewards followed by punishment and vice versa). A therapist can work overtime to develop trust with a Borderline, but the client will ultimately decide when or if that trust is broken, or if it was ever “real.” Building trust through reassurance and altruism with a BPD is like making multiple deposits in an account that never accrues interest and declares insufficient funds when it’s time to withdraw your savings. After all, an untreated person with BPD consistently feels like they’re grieving a vital loss of connection, so they disproportionately side towards subtraction when their all-or-nothing cycle comes full circle. The Borderline’s performative paranoia is unavoidable—even the most innocuous comments or gestures can trigger fears of rejection. The resulting devaluation may include verbal attacks, physical assault, reputational violence, legal threats, and other forms of angry retribution as their self-fulfilling prophecy of abandonment continues unabated. Most disturbingly, people with BPD are unable to recognize the unreasonableness of their behavioral discharges during or after contentious interactions, even if they struggle with guilt or embarrassment. Memory and composure collapse because they’re reacting in an altered state. Shame is avoided by projection. Bad feelings are disowned by demonization. What cannot be integrated must be eliminated. Destruction galvanizes the Borderline’s sense of power, and power is affirmation of their existence.
“Borderlines display a signature trait, poor observing ego, which is a dense denial of vital aspects of reality and irrationality to a degree that almost has to be seen to be believed,” says Dr. Daniel J. Zimmerman. Identity disturbance is evidenced by the BPD’s intense and tumultuous attachment to their love object. They yearn for affection, yet may eventually wish to destroy their love object, or significantly devalue the person’s life. The gratifying sensation of vengeance makes resentment feel justified as the “bad” parent is symbolically punished in a dramatic fort/da reenactment. In order to protect themselves from unbearable disappointment, the Borderline will attempt to regain a sense of control over what they perceive to be an invalidating experience (impulsive BPD subtypes with antisocial features are particularly prone towards destructive recrimination whenever enmeshment is threatened). The angry-impulsive child is experienced by the BPD’s intense rage that is rooted in childhood resentment for not receiving proper parental care. Borderlines must feel a sense of control over others, and they’re easily capable of destroying what they cannot have. The beauty of shared experience is reduced to a competition for supremacy.
“The spoiler child refuses to grow up, remains dependent in some way on the parent or a parent surrogate, and ruins and/or denigrates everything the parents try to do for them,” states Dr. David M. Allen. “The spoiler role is difficult to maintain, so the child needs to continually practice it with other people. The usual candidates for them to practice on are lovers, spouses, and of course therapists. No one else will continue to put up with them.” The phrase no good deed goes unpunished has come home to roost.
The end may justify the means, as long as there is something that justifies the end. — Leon Trotsky
Borderlines often reframe events for advantageous and protective purposes, but retrospective discrepancy identification will separate what’s true from what’s exaggerated or false. People with BPD are poor historians, because the past is written on the pages of their emotions. Facts are replaced by feelings, and a Borderline’s feelings are diffuse. The arc of chronology is contested by the Borderline’s perceptual distortions in such a way that removes fault on their behalf. Confronting and coping with feelings of shame is not going to happen on a BPD’s dysregulated watch. Part of this disorder includes the person’s inability to see their obsession with control and emotional reasoning as disordered. For the Borderline, what feels right must be right! People with BPD seek immediate emotional relief, even if their relief-seeking behavior is irrational, dangerously impulsive, and irreparably consequential. Borderlines do not see their part in causing or contributing to their problems, because admitting such agency would require an uncomfortable awareness of unresolved emotional wounds and a dreaded sensation of humiliation. Likewise, people with BPD believe that most of their problems in life are caused by external factors because they cannot sit with themselves long enough to accept what they’re forever running away from.
Therapists will ignite wildfires of neediness if they try too hard to soothe a Borderline’s emotional flames—transforming themselves into volunteer firefighters searching for the next batch of smoke. Doing too much for these patients inevitably results in causing unintended harm (the Hippocratic oath is eventually replaced with hypocrisy by proxy) because Borderlines don’t know what’s best for them. BPDs must learn how to make the unconscious become conscious, and they must accept responsibility for the unreasonable demands they place on others to avoid abandonment. Otherwise, they’ll perpetually seek enablers and forestall maturation. Remember, Borderlines are living in a state of arrested development and will overreact like unmanageable toddlers whenever confronted with emotionally challenging situations. Outlandish accusations of imaginary crimes and self-justified reactions fueled by animosity can occur in relation to minor inconveniences, innocuous comments, facial expressions, and basic misunderstandings. As a reminder, defiance is not indicators of self-reliance. The need for enmeshment comes from dependency, and the fear of losing enmeshment is offset by internalized or externalized aggression. People with BPD see the world in terms of love and war, because there are no shades of grey on the Cluster B color wheel—it’s a fixed mindset without middle ground. Borderlines would rather be in control than held accountable, and winning is more important than self-reflection (accountability should encourage growth rather than serve as a punitive measure). If the therapist feels responsible for the Borderline’s acting-out behaviors, they will put themselves in the impossible position of becoming a designated babysitter (parentification of the provider). However, reparenting is an impossible task for most caretakers, especially when working with combative adults who gravitate towards learned helplessness. Because of their immaturity, people with BPD do not recognize the line of demarcation where their needs end and another person’s needs begin. Assuming that Borderlines are receptive to rational compromise is an erroneous assumption. Normalizing or minimizing the abnormal, however tempting, is the most fatal decision a mental health clinician can make. Professional integrity depends on recognizing the parameters necessary for self-preservation.
“Psychoanalysts view borderline personality as arising from failure by the patient’s mother to foster coherent differentiation between self and object in the first 18 months of life, leading to the development of pathologic ego defenses. The patient does not learn to tolerate negative effects associated with separation; this continues the child’s clinging into adulthood, as if others were desperately needed parts of the self. Sexuality and dependency are confused with aggression. Needs are experienced as rage. Long-term relationships disintegrate because of an inability to find optimal interpersonal distance. Because of inadequate ego mechanisms of defense, there is little ability to master painful feelings or to channel needs or aggression into creative outlets. The patient has a fragmented mental picture of the self and views others as all bad and simultaneously all potent, a chaotic mixture of shameful and grandiose images,” states Dr. James E Groves.
There’ll be someone else where you used to be; the world don’t care and yet it clings to me. — Tom Waits
By using whatever means available, the focus of all future concerns will be relocated to the Borderline’s elaborate amphitheater of victimhood, thereby disabling all possibility of introspection and responsibility. Misfortune solicits sympathy from others, no matter how much of this misery has been manufactured by the sufferer’s unyielding style of dependency. According to the binary mindset of a person with BPD, you’re either for them or you’re against them. The patient’s desperate longing to use the therapist for positive mirroring has created an unexpected house of mirrors. It’s a peculiar gambit that occurs unconsciously for the Borderline: “I have successfully transformed you to serve my needs, but I will use this transformation against you for rejecting me.” An old country song creeps into the frame: I turned the tables on you, now I’m eating your food. The script has been flipped and DARVO (deny, attack, reverse victim and offender) is the gold standard by which competing narratives are adjudicated. The Karpman Drama Triangle has been played out by two participants on auto-repeat until the rescuer could no longer afford the electricity bill. Unfortunately, the very act of rescuing a Borderline reinforces their early experiences of abuse. Reminders of parental neglect become inevitable when the rescuer fails to match the BPD’s benchmark of idealization. Keeping up with a Borderline’s endless search for emotional satisfaction is impossible, and making customized adjustments to fulfill these unwavering desires only facilitates regression. The therapist, no matter how personally compromised, ethically unmoored, or professionally misguided, will eventually be considered part of a syndicated rejection conspiracy. Borderlines own copyrights to the phrase: “It’s you, not me!” This risible act of projection restores narcissistic equilibrium in the patient while protecting them from unbearable emotional injury. Accepting responsibility for decisions and behaviors is not part of a Cluster B’s externalized game plan. What was once an ideal caregiver for the clinging child has been cast down as an untrustworthy demon who must be annihilated by the punitive parent (talionic revenge). The “omnipotent” therapist now represents the personification of everyone who has previously disappointed and abandoned the Borderline, and the rescue enactment becomes the countertransference equivalent of a head-on collision with an oil tanker.
As intensified rage propels the BPD patient down a seek-and-destroy warpath, the chances for conflict resolution are nil (some Borderlines internalize their rage rather than externalize; others do both). The Borderline’s polarized thinking, projection, dissociation, paranoia, amnesia, capacity for mendacity, and knack for revisionism are the perfect building materials for constructing a gaslit firewall to make sure that accountability will always be a one-way street. Confabulation reduces the pain of mortification and loss. Deny and project; rinse and repeat. Because they were hurt in the past, a person with BPD will do just about anything to avoid feeling hurt again. In the Borderline’s extensive collection of defensive battle maneuvers, there is none more famous than blame-shifting. If they can’t change their environment, they’ll blame their environment (some Borderlines blame themselves, depending on the circumstances). Generally speaking, accepting blame subconsciously reminds the Borderline that they’ll be ridiculed, reprimanded, or punished by their most abusive parent, so the conditioned fear response is projection. High-conflict Borderlines, in particular, will blame others for their feelings, decisions, behaviors, and unhappiness (aka “persuasive blamers”). Anyone who becomes emotionally attached could be blamed for the Borderline’s dysphoria, and anyone who tries to make their life better may suffer a similar fate. Someone must pay for the BPD’s past, present, and future! There are no limits to these disturbing deficits in self-awareness, because Borderline Personality Disorder is a disorder of the self. Disappointment will not be tolerated, and blame-shifting erases feelings of shame, guilt, and humiliation. If the therapist fails to maintain such impossible standards of care, the BPD could lash out with the ferocity of a wild animal if panic and rage pushes them into a collapsed realm of dissociative F2 psychopathy. Someone unrecognizable has emerged. Lifeless eyes, black eyes, like a doll’s eyes. Welcome to the howling abyss. Who is this person? How could the paragon of love and affection so quickly become the personification of hate? But, you see, this “other person” was always lurking beneath the surface. The switch has been flipped; welcome to the split. A horrified child has been awakened in the rejection-rage contingency region. In a metaphorical sense, this is where the clinical exorcism has gone wrong. The therapist has uncovered something raw, and now it wants out of its cage. Primal fury and terror are being released without restraint (the irresistible impulse). The Borderline’s reactivity serves to protect their fragile ego, but it also exposes it.
Retaliatory fantasies may become a reality whenever reality comes crashing down on the Borderline; the emotionally helpless victim transforms into an emotional terrorist. For some Borderlines, their episodic meltdowns are so intense that they literally black out from rage. To make matters worse, rejection sensitivity may result in reactive psychosis when coping mechanisms for stress management are absent. Paradoxically, people with BPD often feel conflicted about their behavior after their dissociative frenzy finally subsides, but emotional memory blocking allows for revisionism and post-hoc rationalizations. However, collapse results in rumination, and rumination often results in abandonment depression. In other words, BPD outrage is eventually reshaped into resentment and carried over into future encounters, thus resuming the cycle. Borderlines sabotage the things they want most in life because they believe that it’s the responsibility of others to make them feel complete—a job that cannot be sustained by anyone. Creating an enemy is how BPDs avoid the fact that they are their own worst enemy (externalize what cannot be realized). Borderlines punish those who act as surrogates for their parents, which means they’re symbolically punishing their family of origin through intimate relationships. For people with BPD to consider: Threatening someone to love you is probably not the best strategy for long-term relationship success. For clinicians to consider: Allowing yourself to become a human punching bag will result in your own need for relational trauma therapy. It’s not enough for Borderlines to be discouraged by unfulfilled expectations, such disappointment means they’ll spread this surplus of misfortune to their object of opprobrium (the abandoner) while using the leftovers to secure new sources of sympathy. It’s a heads I win, tails you lose situation for caregivers. Unreasonably impatient in their wishes for emotional fulfillment, a familiar pattern is repeated. For the Borderline, the mistakes, misunderstandings, and limitations of others are intentionally designed to cause them pain. After all, it’s what they’ve learned from childhood (no one cares; love is a cruel illusion; people cannot be trusted; and the world is a dangerous place). Borderlines falsely believe that everyone hates them, but the reality is that they have learned to despise themselves. Self-hatred was taught to them at a young age, and this hatred will be projected onto their nearest and formerly dearest recipient. In keeping with counterintuitive time, animus makes the sufferer believe that their object of derision is still an essential part of their life. Squaring the circle of Borderline determinism doesn’t make the circumference any less chaotic.
“The BPD’s perceptiveness and knowledge of unfair rules of interpersonal play make her capable of shredding the therapist’s confidence and effectiveness. Her neediness and identification with abusers drive her to ruthless extremes with the therapist. For example, a BPD may detect and appeal to the therapist’s need to be seen as a loved and lovable person. She will offer presents, ask to go to dinner, bring a bottle of wine to the session, plead for hugs and kisses, draw the therapist into confessions about his or her personal problems, and so on. If the therapist appropriately refuses to accept these offerings, he or she is called ‘uptight, cold, uncaring.’ On the other hand, if the therapist accedes to any such gestures, he or she is ‘dead meat’ at a later point in therapy when the BPD is angry about the inevitable perceived abandonment. After desperately and skillfully pleading with the therapist to allow such intimacies, the BPD is completely capable of switching to the following: ‘You violated standard professional ethics when you . . . and I am going to [see a lawyer/call your wife/tell my husband/kill myself and leave a note explaining why].’ It is at this point that a therapist can really ‘lose it.’ We therapists are vulnerable human beings. BPDs are victims who have learned the tactics of abuse, and they are willing to use them on caregivers. The BPD is addicted to empathy and nurturance, but it is vital that such support be given in the service of good functioning rather than in service of chaos, misery, and regression. No matter how lethal the verbal attacks, or how seductive the offers from the BPD, the therapist should hold to the basic terms of the therapy contract,” according to psychologist Lorna Smith Benjamin.
I was a peripheral visionary. I could see the future, but only way off to the side. — Steven Wright
What was once believed to be legitimate desperation during a crisis is now seen as pervasive patterns of emotional dependency and catastrophizing. What was formerly considered to be justifiable anger derived from victimization can now be interpreted as ongoing manifestations of low distress tolerance, repetition compulsion, separation anxiety, morbid jealousy, and emotional reactivity. What appeared to be moments of confidence, moxie, and intellectually justified defiance can now be understood as compensatory grandiosity, antagonism, poor impulse control, and a lack of boundaries. Displays of youthful exuberance, punctuated by periods of terrifying tantrums, have been identified as forms of age regression and emotional instability. What was once thought to be situational anxiety is now understood to be a combination of fear, insecurity, and paranoia. Demands for validation and intimacy have been providing cover for an overwhelming fear of abandonment. An inability to recognize the needs and limitations of others is now exposed as object inconstancy and solipsism due to inadequate mentalization, poor socialization, and insufficient theory of mind. Unpredictable mood shifts are retrospectively linked to the patient’s perceived levels of gratification or disappointment during interpersonal interactions. Passion inundated with tension signifies an inability to manage aggression. Idealization and devaluation are explained by the client’s Manichean mindset and zero-sum approach to relationships. People and situations are rearranged to fit the emotional reasoning of the Borderline to obtain a sense of safety and control. Destruction is justified by perceived rejection. What was once a victim of abuse is now an agent of abuse. The acronym FOG is appropriate because fear, obligation, and guilt create a haze of confusion until the experience of interacting with a Borderline patient is analyzed long after the chaos has cleared.
Blessed is he who expects nothing, for he shall never be disappointed. — Alexander Pope
Borderlines tend to remember others based on their last encounter: The Great Moment of Disappointment. Everything that was previously done to indulge the BPD’s demands for special consideration will suddenly be forgotten, because holistic integration of interpersonal experiences do not register for this uncompromising competitor. The therapist has been serving as the Borderline’s stabilizing crutch, and removal of that crutch exposes a painful disability. Exposure = death of the false self, which is experienced by the Borderline as a form of biological death. And, if the person suffering from BPD has a “high splash” response when triggered by fear and frustration, there will be hell to pay. To be sure, their formerly cherished caregiver will be left holding the tab. The Borderline’s hypervigilant surveillance system obsessively scans for potential insults, slights, disagreements, and signs of rejection to maintain a self-fulfilling panorama of paranoia. Everything is personal, and they’ll interpret any inconvenience or change of plans as a form of deliberate abandonment. The slightest mistake or misunderstanding will be interpreted as a global catastrophe. Deflection and projection; impulse and emotion; passion and punishment; grievance and resentment. BPDs do not have the ego strength or maturity for compromise, and their tenuous image cannot endure mortification. Without compassion for themselves, there will be no compassion for you. Informal resolution is not on the Borderline’s menu, because they demand absolute control over the final narrative. A BPD must reject facts and information that counter their feelings, because emotional convictions cannot be contested. The better the fuel, the harder the fall. Grudges never die easily for Borderlines. And don’t expect to get credit for your generosity, empathic consideration, or accomplishments. Remember, it’s all-or-nothing, no matter how many times you’ve given it your all. In the Borderline’s mind, your beneficence was disingenuous, insufficient, or a devious plot. Why would anyone care? What’s in it for them? To be fair, Borderlines aren’t aware that such irrationality and destructive overreactions are primitive defense mechanisms to avoid feelings of low self-worth, shame, and abandonment that were formed during early childhood. And, to be clinically concise, the therapist has royally screwed things up because of a failure to see the forest for the trees. A series of clinical mistakes has resulted in a series of personal mistakes. The German language contains a splendid word to describe this type of regret-ridden hindsight: Treppenwitz (a devastating rejoinder thought of only after leaving the bottom of the staircase). You don’t have to be an ophthalmologist to appreciate the excruciating lessons of hindsight. The therapist’s professional miscalculations, poor judgment, lack of specialized training, and personal issues cannot be whitewashed, but expecting the unexpected is par for the course whenever working with Borderlines. Being consistently inconsistent is what makes this disorder so insufferably persistent, and sabotaging therapy, as with any other relationship, is just another form of self-sabotage.
“The Brutal Clock is a variation of the Brutal Test where the Borderline sets up impossible expectations of others. When others are unable to meet these unreasonable expectations, they are punished with emotional abuse, which is justified by the Borderline’s sense of being the victim because they did not get what they wanted,” explains Dr. Daniel S. Lobel.
Free will is the internal forces I do not understand. — Marvin Minsky
A gnawing question remains: Are the Borderline’s cataclysmic reactions to real or imagined abandonment intentional or purposefully malicious? No, not in any normal sense; exceptions involve high comorbidity or subclinical constructs with behavioral traits of vulnerable narcissism, psychopathy, and BPD—aka the vulnerable dark triad (VDT). For example, a propensity for criminality is indicative of a “malignant borderline” and may include elements of sadism, narcissistic rivalry, and malicious envy. The confluence of early childhood attachment disruptions, severe psychopathy, other personality disorder pathology, and a traumagenic abuse history are factors that represent the worst recorded manifestations of BPD. PCL-R Factors 2a and 2b are strongly correlated with Antisocial Personality Disorder and Borderline Personality Disorder because they’re associated with reactive anger, criminality, and impulsive violence (frustration is expressed through aggression). Although various traits of psychopathy are present among all Cluster B disorders, antisocial behavior for Borderlines is usually a consequence of emotional dysregulation during periods of acute adversity (F2 psychopathy as a dissociative feature). Although people with BPD usually feel guilty or conflicted after acting out, accepting accountability for the consequences of their actions causes too much stress and shame, so the object of their frustration will ultimately be expected to fall on the sword.
According to the American Psychiatric Association, the prevalence of BPD in correctional settings is typically higher than in psychiatric in-patient settings (about 20 percent), and more than double that of out-patient mental health clinics (about 10 percent). For those suffering from Borderline Personality Disorder, paranoia, panic, anger, impulsivity, and severe dissociation are the primary precursors to reactive rampages. An incomplete, incorrect, and emotionally biased interpretation of reality lights a short fuse that detonates the Borderline’s unhinged behavioral responses. To be sure, interpersonal hypersensitivity is not an explosive device to be messed with by the uninformed. By contrast, there are highly sensitive people who have been misdiagnosed with Borderline Personality Disorder because they self-identified with some of the most common traits (self-report is an unreliable diagnostic metric). Although recognizing BPD traits in themselves, these individuals would not relate to the character portrayal in this fictionalized account. In addition, there’s undoubtedly a segment of Borderlines in treatment who continue to rely on their diagnosis to justify selfish and destructive behavior, but their motivations would be difficult to determine with accuracy. This is where the No True Borderline fallacy becomes relevant. For example, people with BPD will say, “I’ve been diagnosed with Borderline Personality Disorder, but I don’t behave like that; therefore, the person you’re describing is not a true borderline.” By contrast, those who are married to or related to a person suffering from BPD will say, “I’ve lived with a Borderline for many years; therefore, this is how a ‘true borderline’ thinks and behaves.” In the end, we’re left with anecdotes, varieties of subjectivity, factual accounts, misunderstandings, assertions, beliefs, assumptions, informed opinions, clinical assessments, and elements of truth that are lumped into the ongoing BPD controversy. In reality, many things can be true or false at the same time (we’re all on the honor system). So much depends on the storyteller, the situation, historical patterns, and the evidence. People with BPD will tell you what it’s like to be them, and others will tell you what it’s like to interact with Borderlines. Nevertheless, we must admit that no two people are identical. Generalizations are sometimes useful, but the person and the context will always be somewhat unique. Borderline Personality Disorder exists on a spectrum, just like the experiences of those who interact with personality disordered people. That being said, many members of the Cluster B brigade are maestros at invalidating or minimizing the experiences of others, and they consistently maintain denial about their own behavioral inconsistencies.
Borderlines confuse subjectivity for reality because they lack a reality-based ego (the defensive structure of this disorder prevents whole object relations and impairs reality testing). Overall, you cannot reason a person out of a position they did not reason themselves into, and BPD radically changes a person’s perception of what’s considered reasonable. Partners of Borderlines not only feel like they’re walking on eggshells during these relationships, but they also feel like they’re walking on eggshells whenever they attempt to recount their experiences (accusations of cruelty, neglect, and ableism are expected). Nonetheless, there are BPD behaviors, beliefs, and proclamations that repeatedly converge like a broken record. Likewise, many people who interact with Borderlines have witnessed these similarities as if they were choregraphed in advance by the same person; just ask any two people recovering from a BPD relationship. Borderline Personality Disorder follows a trajectory that is identified over time with many universal features, regardless of severity. The key is to recognize these patterns before becoming entangled with the exigencies of the person’s disorder. Diversity among sufferers is not a vindication of the disorder or its negative effects.
If anyone should have animosity towards Borderline Personality Disorder, it should be those who suffer from it. For the most part, people with BPD are hard-wired to impulsively think and behave in ways that allow them to get their immediate needs met. In other words, Borderlines are aware of their behavior, but they’re not aware that their behavior is generated by pathological underpinnings (the disorder prevents them from seeing themselves as disordered). They believe their thoughts and behaviors are justified according to the whims of their profuse emotions. So, it could be said that Borderlines intend to get their needs met; their motivations are unconscious; and their behavior is automatic. Bullying, seducing, pouting, coercing, and threatening others to comply with their desires is how BPDs communicate. Borderlines have learned to dissociate from traumatic experiences, but they also dissociate from the trauma they cause others. Causing pain through punishment—towards themselves or others—is a dysfunctional way of signaling that they’re in pain; besides, it’s all they know. When love is withheld, the world is set on fire. Dichotomous reasoning is most dangerous when “you made me feel bad; therefore, you are bad” determines the Borderline’s range of retaliation. The drama is the point, of course, because mayhem fills the void. Emotional reactivity isn’t privy to the concept of courtesy or having consideration for long-term consequences. Most Borderlines have low distress tolerance, but some people with this disorder have no distress tolerance. Another Borderline paradox: BPDs live in a state of distress; identify with distress; expect distress; create distress; but they cannot cope with stress. As a general rule, the survival of the Borderline will overrule the survival of anyone who gets in their way. Being less than perfect was usually not permitted during the BPD’s childhood, so someone else must fall on the sword whenever future “mistakes” are made. Disproportionate reactions to misunderstandings or perceived threats often result in destruction without compunction. You’ll be punished for not maintaining your role in the BPD’s theater of need; but don’t take it personally, it’s just Borderline business. However, the incalculable damage left in the wake of their rage will feel very personal. Hurricanes destroy lives because natural disasters lack self-awareness and restraint. To be sure, Borderlines are the heavyweight champions of emotional storm systems.
The long-awaited one has come; I ask nothing more of the sea. — Madame Butterfly
A musical analogy for therapy-patient relations gone wrong with a Borderline is the ebb and flow of symphonic development. In other words, the therapist’s efforts to appease the BPD were constructed from variations on a simple motif: You are worthy of being loved. Unfortunately, proof of love for the Borderline is contingent upon reassurance, unrealistic expectations, and commanding the will of the therapist to avoid facing the pain of their inner experience. The tempo of the second movement is similar to that of the first, but subtle changes in dynamism make it more consequential than it may at first appear as the call and response of melodic interplay becomes crisis and reaction. The evolution of this unsustainable saga results in a rapid crescendo of dramatic fusion during the third movement towards an ecstatic final stanza. As with therapy, it’s never a single session, but a series of misguided steps over many sessions that move incrementally before resulting in a complex web of enmeshment that has to be unraveled as painstakingly as it developed. Unfortunately, the Borderline demands loyalty and insists on maintaining the emotional intensity of the third movement. If the magnitude of the emotional bond is not maintained, the performer (therapist) will be punished by the BPD who feels immense anger for the abandonment of a quixotic attachment. The therapist, who unfortunately became a volunteer performer in the Borderline’s theatrical search for devotion, forfeited the conductor’s role of mediating between order and chaos. As a result, the therapist has subverted the structure of the compositional (therapeutic) framework, and the disheartened BPD patient has unleashed a cyclone of emotional turmoil throughout the concert hall.
“Specific transference-countertransference enactments are at high risk for occurring with patients with
borderline personality disorder. If a patient has experienced neglect and abuse in childhood, he
or she may wish for the therapist to provide the love the patient missed from parents. Therapists may have rescue fantasies that lead them to collude with the patient’s wish for the therapist to offer that love.” — (excerpt from Practice Guideline for the Treatment of Patients with Borderline Personality Disorder)
*It’s important to respect your rhythm instead of trying to keep up with the tempo of a Borderline. In other words, therapists should concentrate on reducing the patient’s “beats per minute” rather than meeting them halfway or becoming swept away by their impulsive speed of need. Keeping pace with Borderline time is unsustainable—it’s the accelerated rhythm of hypervigilance—and the frenetic pulse will burn out even the most measured of metronomes. Borderline entrainment is a fast-moving train, and it’s best for therapists not to leave their station.
Assumptions held by BPD sufferers (according to bpdcentral.com):
Absence is a house so vast that inside you will pass through its walls and hang pictures on the air. — Pablo Neruda
At the end of the abandonment rainbow, the disillusioned Borderline will be encouraged by sympathetic allies to collect misadventure points while reclaiming victimization. However, the clinician will suffer a much greater loss because professional boundaries were not clarified before sauntering into such a formidable therapeutic landscape (countertransference errors are much more likely to occur whenever a patient is undiagnosed or misdiagnosed). The path by which any therapist deviates from protocol can be retraced, fittingly, by understanding how mysterious the realm of human psychology can be during unorthodox encounters. Patients with characterological disorders can elicit out-of-character responses in their clinicians. All therapists have professional blind spots, biases, and personal weaknesses, but there is, perhaps, no patient better at uncovering those blemishes than a Borderline. BPDs are instinctively searching for the ultimate caregiver to remove intolerable feelings of emotional pain leftover from unresolved childhood wounds, and they will go to great lengths to make this fantasy come to life. For historical clarity, the distinction between pervasive patterns of behavior versus circumstantial aberrations must be identified for all participants.
“We often think of boundary violations and therapist misconduct as being malevolent in nature,” Dr. Bryant Welch writes. “But with a borderline patient, a therapist can get into trouble by virtue of his or her wish to help and have a therapeutic effect. Under enormous pressure to prove he or she ‘really cares,’ the therapist is either going to cross boundaries and/or ‘withhold,’ thus becoming a ‘bad object.’ The grounds are fertile for BPD rage and disappointment in either direction.”
You just keep me hanging on. — Lou Reed
Rationalizations and promises often emerge in direct proportion to the Borderline’s increasing demands for validation and reassurance. BPDs need someone to lean on, but too much safety rope given to a clinging client can eventually become the noose that hangs the therapist. To add insult to injury, it’s embarrassing for any therapist to admit that they’ve become emotionally ensnared with a mental health patient as a result of clinical misunderstandings, communication errors, insufficient boundaries, and trauma bonding. Like a surgeon who encounters complications in the operating room, the very act of trying to remove a person’s suffering can sometimes exacerbate it. Many therapists have too much pride in their abilities to call for backup, but backing out of Borderline Boulevard is never an easy ride—there will be damage. The margin of error is very narrow for making clinical errors with a BPD, because forgiveness is not part of their reactionary repertoire. Replacing the parts as they break (“fixing” the symptoms) will never repair an engine that needs to be rebuilt from scratch. No matter how rewarding the process of empathic appeasement may feel for caregivers, taking extraordinary risks to accommodate a patient’s needs is not the same as encouraging them to establish their own sense of equanimity and independence. Becoming too involved with someone who self-sabotages in relationships is itself a form of self-sabotage. Borderline Personality Disorder is a matter of principle and implication. If the therapist understands the principle, they’re in a better position to handle the implications; if not, they’re likely to become a casualty of those implications.
Forgiveness is the fragrance that the violet sheds on the heel that has crushed it. — Samuel Clemens
Specialized training programs to diagnose, effectively treat, and facilitate the management of Cluster B pathologies should be mandatory as a preventive measure to avoid Type II errors in assessment and countertransference disasters. There are more than 200 classified forms of mental illness with notable differences in presentation, and no clinician is an expert on treating and understanding everything. The human mind is a strange place, and it becomes a lot stranger as therapists learn more about themselves while attending to the maladies of their patients. Respecting commonly understood boundaries among adults who consent to therapeutic contracts is usually taken for granted, but it’s not guaranteed during emotionally complicated and confusing clinical encounters. It’s up to the therapist to understand the importance of defining clear limits at the beginning of therapy while being intrepid in the face of aggressive boundary testing. Recognizing clinical shortcomings; admitting personal issues; seeking consultation; and following ethical guidelines will ensure a professional relationship for the sake of everyone’s well-being. Similarly, it’s up to the Borderline to courageously work on developing insight by understanding how a lifetime of dependency and defensive reactivity prevents developmental growth and behavioral accountability. In cases involving ineffectual or destructive therapeutic dyads, understanding what went wrong should be given far more significance than determining the correct calculus of blame. We are all products of our genes and our environment. Some of us are profoundly unlucky in the lottery of life. No matter how hard we try to escape the past, we can never fully escape our vulnerabilities. Motivated by misapprehensions and a desire to indulge the client’s desperate need for human connection, the therapist became an enabler rather than remaining a professional guide. When working with well-documented BPDs, analyzing should never yield to appeasement; confronting should never yield to catering; and challenging should never yield to capitulation. However, when working with an undiagnosed or misdiagnosed Borderline, good luck trekking through those enigmatic eggshells (armchair deductions writ large). Ultimately, therapists who remain committed to pleasing others need to practice saying “no” whenever their client’s needs become overwhelming. Patients with BPD will not respect a therapist’s sacrifices, they’ll learn to expect them. Sacrificial gestures become nothing more than a transactional endeavor that circumvents self-awareness, emotional discomfort, and the process of change. There are no shortcuts. Borderlines want others to acknowledge their vulnerabilities, but their mindset is not equipped to fully contemplate the vulnerabilities of others. As Dr. John Gunderson reminds us, clinicians who work with Borderline patients must have an extensive knowledge of this disorder; adequate experience working with this disorder, and an actual desire to treat those suffering from this disorder. Likewise, those who try to help a person with BPD the most may be the ones who suffer the most consequences, especially if they’re not informed and prepared in advance. The most consequential clinical encounters occur when the Borderline patient’s desire for an unambiguously gratifying, “all-good” mother collides with the therapist’s desire to be seen as an “all-good” caregiver. The wish to fuse with the mother for emotional nurturing must be endogenously generated by the Borderline rather than externally sought, controlled, and tormented whenever this longing is frustrated.
“Working with patients suffering from borderline personality disorder begins with an acceptance that they live in an immature psychological world, fueled by certain constitutional vulnerabilities, where they attempt to shield themselves from conflict and anxiety by splitting the world into all good and all bad. Although this produces an illusory sense of psychological safety, in fact, it renders relationships fragile and chaotic and drives away the very people who are so badly needed to stabilize the patient,” states Dr. Marcia Goin.
Now that my ladder’s gone, I must lie down where all the ladders start, in the foul rag and bone shop of the heart. — W.B. Yeats
For better or worse, the therapist will realize that being a caretaker, despite the best of intentions, cannot include the responsibilities of completely taking care of another adult. The three Cs need to be reviewed: The therapist did not cause it; the therapist cannot control it; and the therapist cannot cure it according to the Borderline’s unrealistic expectations. Consolation should be the fourth C, and it’s never enough for a Borderline. Becoming a surrogate parent, unfaltering friend, love object, support structure, or omnipotent rescuer to save someone from a lifetime of dysphoria is a recipe for disaster. There’s no pier strong enough to stabilize The Great Ship of Desperation. The therapist will need a bigger lifeboat to endure the Borderline’s self-generated waves of fear. No single individual can successfully meet all of the emotional and physical needs of another. Being supportive, empathic, and comforting should never drift into the realm of everlasting availability. Likewise, Borderlines should be discouraged from providing transference-based gratification to their caregivers by association. The ephemeral anodyne of validation may satisfy the desire for human connection on both sides of the couch, but therapists may never find their way back once the process of BPD pacification begins. If a clinician falls off the Cluster B tree early on in the therapeutic process, they’re likely to hit every countertransference branch on the way down. When all is said and done, the therapist cannot invoke the Nuremberg excuse: I was only following orders. Codependent quicksand is a formidable force.
A Partner’s Perspective The only one for me is you, and you for me. — Alan Lee Gordon
There’s much debate regarding the term codependency and the popular idea that all individuals who become intimately involved with a person suffering from Borderline Personality Disorder are essentially “codependents.” Codependency being defined as excessive emotional or psychological reliance on a partner, typically one who requires support on account of an illness or addiction. Basically, someone who is considered codependent, especially in terms of a BPD relationship, is someone who is willing to take on an excessive amount of responsibility for their partner while attempting to “fix” their problems. A person who is codependent will also relinquish his or her own needs and wants to care for another person. However, Codependent Personality is not recognized in the DSM because codependency is considered a non-clinical psychological construct. Furthermore, human psychology is a soft science that does not allow for all statements or any declaration that demands 100% certainty; to suggest otherwise would be committing the fallacy of illicit transference. Although common pairings in borderline relationships involve partners with Narcissistic Personality Disorder and nominal codependents, there are plenty of healthier-minded individuals who find themselves caught up in BPD relationships before understanding anything about the disorder—sometimes several years after the relationship has ended; sometimes never. In many cases, the partner of a Borderline has tried everything at their disposal to make the relationship work until a combination of confusion, frustration, exhaustion, and unexpected fallout forces a contentious separation—the personal, social, and financial burden can be enormous. Short-term appeasement to the BPD mindset could, in some cases, be testimony to a partner’s patience, concern, compassion, commitment, love, and resilience rather than a tendency towards codependency. In fact, the most common tendency among partners of people with BPD, especially during the early stages of a relationship, is to view this type of suffering as peripheral or temporary rather than pathological. Interpreting and managing a Borderline’s unpredictable moods, while simultaneously attempting to solve the riddle of object inconstancy, would be counterintuitive and difficult for anyone (add a dash of identity diffusion for extra confusion). More often, the Borderline’s episodic dysphoria, abandonment anxiety, learned helplessness, and constant need for reassurance are the primary sparks that trigger the codependency time bomb, which, like BPD, should be evaluated on a spectrum.
It’s worth remembering that a person with this disorder seeks external regulation through an intimate partner who also serves as a surrogate parent. Consequently, this relational need becomes an existential imperative that causes myriad mistakes in communication and interpretation. Another mistake occurs when partners try to simplify this complicated disorder by becoming crisis custodians—believing that each crisis is fixable rather than enduring. Partners of people with BPD often describe themselves as full-time doormats and punching bags; prone to argumentation due to aggravation, or acting in unusual ways that only occur in the context of the relationship. Many individuals stay locked in these relationships because Borderlines will assert, in no uncertain terms, that their partner has the cure for what ails them (i.e., love, special assistance, and emotional support). These assertions are usually so compelling that many partners of BPDs will work even harder to “do better.” When creeping codependency is misinterpreted as love, the hedge maze of misguided compromise begins to obscure all exit signs leading to healthier perspectives (both partners eventually drown in a morass of impaired reality testing). Furthermore, because love is neither sufficient nor effective for ameliorating the wounds of this disorder, a deeper hole is being dug on a daily basis by the supplier. Along the contours of counterintuitive encounters, BPD is the type of disorder that compels uninformed partners to cater to it without knowing what’s occurring.
Most people enjoy being idealized and most partners of Borderlines will try to live up to the image created by the donor of such extravagant encomiums. Let’s face it, it feels good to feel needed, and it feels even better to improve someone’s life through acts of devotion, compassion, and generosity. Conscientious people do not want to disappoint those in distress, and tolerance develops through adversity (culture reinforces the idea that we should never give up on committed relationships). Unfortunately, the source of a Borderline’s gratification and stability inevitably becomes the source of their unhappiness and resentment. Over time, their preferred support system will run out of energy and resources. When this happens, the person with BPD will angrily assert that their partner never really cared or loved them. In fact, clinical depression, apathy, alcoholism, health problems, chronic fatigue, premature aging, and C-PTSD are common among current and ex-partners of Borderlines because of the cognitive dissonance and chronic stress involved with the roller-coaster nature of these relationships (similar problems can occur for adult children of Borderline parents). There’s nothing breezy about a BPD relationship; once things get going, they become firestorms without reprieve. For some partners of Borderlines, the fawn response is conditioned in correlation with their repeated attempts at de-escalation. Demands for time and attention that were originally accompanied by adoration soon give way to criticism, belittling, and increased agitation. The test that a person with BPD administers for loyalty is neither meant to be passed nor entertained, and taking this exam is volunteering for punishment. To walk in the shadow of shame is often the end game for partners who promise to provide relief—willing to drop everything at a moment’s notice—for their incessantly distraught counterpart (play unwinnable games and win regrettable prizes). On the whole, these relationships are logistically unworkable, internecine, and involve various stages and phases that become cyclical for the sufferer. Too much involvement promotes learned helplessness and too little involvement triggers separation insecurity. As if that wasn’t difficult enough, there’s no referendum on a Goldilocks Zone. Those who are unfamiliar with stability don’t know how to relax and accept it without misgivings whenever it’s on offer. Sadly, no one distrusts the process more than a Borderline.
For a someone to fall in love with an untreated Borderline essentially means that they’re falling in love with someone who hates themselves. Subsequently, the self-hatred of the disordered will be projected onto their partner during periods of emotional turmoil. BPD “meltdowns,” which usually involve splitting, have the power to melt mountains. Nuclear reactors could benefit from attending a BPD lecture series when it comes to maximizing radioactivity. When the sufferer’s rage supersedes the melting point, the anxiety, fatigue, and disorientation it causes for their partners is inescapably detrimental. There are documented cases of partners being physically assaulted by their BPD spouse or lover with weapons of opportunity during heated arguments; committing suicide from prolonged exposure to borderline abuse; losing their reputations and livelihoods; losing their sanity; experiencing long-term legal consequences, or having their lives ruined in some manner that defies comprehension. Ex-partners may experience distortion (smear) campaigns, false allegations, legal retaliation, harassment, stalking, and other acts of obsessive revenge; sometimes months or years after contact has ended. In the most extreme case examples, murder is on the menu. The most important thing to remember about frantic attempts to avoid real or imagined abandonment is that they’re frantic. There are no limits to what can happen when a Borderline’s emotional supply source is cut off. If allegations contain some element of credibility, they’ll often include paranoid misunderstandings, exaggerations, confabulations, lies, catastrophizing, gaslighting, and an astonishing lack of accountability (the cathexis of projection disables meaningful insight). Whenever vindictive behavior is enacted, it’s believed to be deserved as an appropriate punishment for the fabricated felony of abandonment in a Cluster B courtroom of unappealable emotional conviction. Generally speaking, Borderlines do not take ownership of their uncompromising neediness and its devastating effects during periods of acute stress. Because the person with BPD presents differently in public than behind closed doors, and because the nature of their disorder is highly counterintuitive, explaining such surreal shenanigans and trying to convince others of the truth will likely be met with disbelief.
Borderline abuse is distinct from but very similar to narcissistic abuse, and it occurs reflexively through intimate interactions. Relationships with untreated Borderlines are essentially anachronistic, sado-masochistic, and coercively codependent. The person with BPD conflates dependency with love and then justifies continued dependency by assigning nefarious motivations to anyone who “insufficiently” supports (enables) or disavows (abandons) them. What transpires is a harrowing pattern of parentification and vilification; neediness and resentment; expectations and disappointment; praise and punishment. Borderline abuse is basically a byproduct of the sufferer’s need for control, but people with this disorder feel very strongly that their behavior is justified in each moment. There are three primary areas of abuse that a BPD’s partner will experience as a natural consequence of the sufferer’s pathology:
Some partners of Borderlines become equally abusive when they can no longer suppress their own anger, anxiety, and frustration (reactive abuse); others are berated into submission (freeze response) or find “inventive” ways to escape the trauma of the relationship (i.e., distancing, ignoring, dissociation, addiction). Giving up based on sheer exhaustion is normal when the fighting, salvo of insults, screaming, circular conversations, and drama never ends. To say that a lack of motivation on the partner’s behalf is correlated with a precipitous decline in relational rewards is a massive understatement, because most statements made by an aggravated Borderline are loaded with critical and abusive language. This is why Borderline Personality Disorder is sometimes referred to as a “disordering disorder;” because anyone who gets too involved in the sufferer’s life becomes disordered by association. In this sense, the disorder becomes a psychological contagion with a high infection rate; reconditioning their partner’s nervous system to a similarly dysregulated state. To add insult to injury, or just more injury, any pre-existing problems of a BPD’s partner (health, financial, occupational) will be made exponentially worse by the dynamics of the relationship. Furthermore, a delayed onset of the most telling diagnostic features can appear long after these relationships have been consolidated by cohabitation or marriage. Most individuals rationalize warning signs while intoxicated by the early stages of companionship, and no one is immune to making interpretive mistakes about another person’s character. Red flags evolve incrementally and are frequently excused without further appraisal by those who are forgiving. With this type of disorder, it’s difficult to comprehend the disturbance of the sufferer until their partner makes the error of normalizing the relationship. Wanting to think the best of the person without understanding BPD, their partner will bestow qualities of character and cognition upon them that are not commensurate with factual information. A great deal of disbelief in the sufferer’s capacity for instability and conflict comes from witnessing the Borderline’s better behavior while being wooed by the ornate parameters of their false self. The exhilarating allure of intense positive emotions among people with this disorder results in captivation and misdirection until they suddenly burn the house down after becoming emotionally overwhelmed. To say that the Borderline’s partner “allowed” the relationship to develop is technically true, but it’s experientially inaccurate. There’s a compelling immediacy that portends an ensuing power struggle, and each questionable interaction that’s permitted is not understood for its creeping complications. *Consenting to a relationship of any ilk does not imply consent to being controlled and emotionally tormented by another human being, but the ramp of the unforeseen is too often paved with streams of glitter, fool’s gold, and naive optimism. Being enthusiastically wrong about another person’s character gives rise to a disorienting leap into the unforgiving terrain of impaired reality testing.
In a quest to break the irony meter, BPD pairings on the upswing have a way of encapsulating the most desirable qualities of human connection, only to produce the most undesirable qualities as the connection progresses. The partner of a person with BPD is initially designated as someone who can do no wrong until they can’t do anything right. Idealization followed by devaluation causes partners of Borderlines to question their own sanity, as they anxiously scramble to get back in good graces. Intermittent positive reinforcement is a powerful incentive that offsets the initial confusion caused by Borderline splitting. Hope is a helluva drug. After all, everything seemed so wonderful in the beginning when everyone was riding high in the Borderline Bubble—a magical place where everything seems perfect; everything is exciting; everything feels safe; anything is possible, and everyone feels loved. To sweep someone off their feet during a whirlwind romance is a natural talent for many people with this disorder, but this also involves sweeping a stockpile of uncomfortable truths under the rug. Reality is repudiated and regression is glorified in an inviting cocoon of fervent symbiosis. The Borderline Bubble (aka Fantasy Preservation Society) is an unsustainable fairytale in search of an unwittingly compliant sponsor, and the incentives are outwardly enticing because Borderlines are especially exciting, sweet, and affectionate in the early stages of a relationship. In fact, some people with this disorder are so impeccably appealing that you’d never image how much they’re struggling inside, or what they’re capable of when triggered. For example, high-functioning Borderlines who are successful in their careers and recreational pursuits can have all of the trappings and affectations of a cosmopolitan adult without anyone knowing they’re saddled with the mental architecture of a frustrated child when interacting with intimate others. Being blinded by the splendor, the BPD’s psychological wounds, developmental deficits, and ongoing internal conflicts are not apparent to the casual observer. It’s worth reiterating that a Borderline’s false self, albeit preferable in its pageantry and tenuous stability, is just another manifestation of their disorder. Being a disorder of the self, the Borderline’s false self is by definition inauthentic and fragile. The partner of a Borderline, in essence, becomes the unsuspecting bird who breaks its neck by trying to fly through a picturesque window. There’s an attraction to a specific set of defense mechanisms (the enchanting side) that inevitably fades when a new set of defense mechanisms (the chaotic side) moves into the frame.
When it comes to Cluster B curb appeal, nonparticipants may ask how a serious mental health condition could receive such rave reviews during its debut? It’s been said that love is blind, but Borderlines have a way of turning their partner’s windshield into the world’s biggest blind spot. Aside from the physical features of the disordered, some partners find the Borderline’s approach-avoidance style of courtship to be playful, challenging, and enigmatic. Some find the Borderline’s childlike disposition to be endearing and their obsession with romantic subject matter equally captivating. Others are attracted to the intensity and drama evinced by people with BPD because it makes the relationship seem larger than life. Many partners become gradually addicted to the Borderline’s emotional rollercoaster and periodic bedroom antics employed to reanimate connection. Natural-born caretakers enjoy feeling needed and falsely believe that their empathy and attentiveness are sufficiently restorative. More often, partners are swept away by the uninhibited energy of the Borderline and find their companionship during periods of elation to be irresistible. Perhaps the most universal mistake among partners of Borderlines is taking their love bombing and mirroring personally rather than identifying these actions as disordered behavior. The secret sauce of pedestalization is that every positive attribute of the Borderline’s partner is amplified to such a volume that reality can no longer be heard, which makes the partner’s past feel like dress rehearsal for the relationship. In addition, partners suffering from their own pathologies or unmet needs may hope to find themselves in the ethereal absence that defines the malady of BPD. Losing oneself in someone else is metaphorical fodder for fairy tales and romance novels, but waking up from the fantasy is the only way to assess how much was really lost after finding oneself on the other side of a Borderline relationship. Collectively speaking, any relationship that revolves around doing someone’s bidding to compensate for their deficiencies is neither reciprocal nor sustainable.
Borderlines place their partners in an unenviable and unsustainable position that requires both regression and parentification. Regression is required to avoid feeling threatened by their intimate partner’s adult autonomy, and parentification is required to ensure continued dependency. The shared fantasy is an intoxicating atmosphere but it requires absolute compliance and superhuman commitment by the partner, and the rules inside this bubble will shift according to the whims of a dysregulated lawmaker. Interference from the outside world is anathema in the bubble because it impinges on the Borderline’s fantasy defenses, so any deviation from this safe space (i.e., separation or disagreement) will be met with frustration, anxiety, panic, and anger. Ultimatums to forestall abandonment may also be accompanied by self-harming behaviors, threats of suicide, or suicide attempts. The idealization phase was nothing more than being temporarily anesthetized in the eye of a hurricane, but the strongest winds are on the horizon. What can’t be predicted is usually what ends up hurting us the most, and no one knows this better than a Borderline (irony makes another comeback). Cloud nine rapidly morphs into a never-ending nightmare as the person with BPD begins to reactivate their traumatic history. In this sense, intimate partners become vulnerable to the vulnerabilities of the Borderline—identifying with their projections, validating their delusions, and endorsing their fears until a mutually magnified “mindfuck” blossoms into a freakishly dysfunctional dynamic that resembles romantic schizophrenia (certified crazymaking). What once looked and felt like an enticing daydream now resembles an abstract hellscape seen during a bad acid trip. Sooner or later, the emotional dysregulation of the Borderline causes their partner to become correspondingly dysregulated as they twist themselves into a deferential mess by attending to a litany of labile moods, emergencies, accusations, and capricious stipulations. Redundant arguments, profligate conversations, nonsensical confrontations, staggering bewilderment, and escalating frustrations begin to fill the anxiety-ridden airspace. To make matters worse, the Borderline’s hypersensitivity to criticism and perceived slights obviates the prospect for constructive criticism during fireside chats (emphasis on the fire). The partner of a person with BPD eventually realizes that they’re spending most of their time trying to explain why certain thoughts are irrational; why certain feelings are unwarranted, and why certain behaviors are inappropriate. As futile as it is compulsive, the acronym JADE (justify, argue, defend, and explain) subsequently becomes a lifestyle.
Some Borderline relationships result in multiple breakups followed by equally disastrous reconnections initiated by a “hoover;” others remain steadfast until the partner finally collapses under the draining burden of accreting madness. In many cases, the Borderline’s fear of engulfment will drive them to preemptively discard their partner with unmatched callousness to avoid the indignity of abandonment, or to locate more accommodating pastures in what can only be described as a romantic pyramid scheme (aka “monkey branching”). Infidelity may be as common in these relationships as wishing that infidelity occurred to justify ending the relationship. When it comes to untreated Borderlines with high-turnover rates in the partner department, their repetition-compulsion cycle produces tidal waves of collateral damage, and anyone left standing in the wake of their kinetic leapfrog legacy is forced to accept the unacceptable. After all, if life is a ruthless competition where no one can be trusted, then intimate relationships should also be expected to tow the crooked line. Romanticize, devalue, and destroy is the only formula untreated people with BPD know they can trust.
All things BPD become easier to digest with a rudimentary rhyme: Borderlines have problems with separation-individuation and they rely on others for emotional regulation. They want to be accepted, loved, and respected, but their capacity for introspection is thwarted by their fear of rejection.
The self-satisfied rejoinder “it takes two to tango” is a bit of a misnomer in these relationships, especially when you consider that a person with BPD experiences multiple dissociative states, rapidly fluctuating emotions, conflicting desires, and wildly inconsistent moods. Identity disturbance is a significant part of the instability package, no matter what constitutes a Borderline’s “baseline.” When it comes to an untreated person with BPD, you’re seldom dealing with the same person, and most of the time they don’t remember what part they played during significant altercations due to switching, splitting, and dissociative amnesia. The relationship itself exacerbates the disorder because Borderline Personality Disorder is a relationship of the self that includes having a bad relationship with oneself. Generally speaking, there’s a Mr. Hyde hiding behind every Henry Jekyll, and every “moment of clarity” or period of stability is inevitably subsumed by a retrograde temper tantrum whenever the person with BPD is triggered. At best, Borderline Personality Disorder represents an unintegrated duality; at worst, it devolves into unadulterated psychosis. To complicate an already complicated mess, the Borderline’s inability to self-regulate or relate to others is usually misinterpreted by their partner as somehow being their fault, and this belief is reinforced because there’s no shortage of blame during acute periods of emotional decompensation. Not knowing where these feelings are coming from, the Borderline externalizes causation with a very broad brush. As if this ballroom blitz wasn’t confusing enough, the plot sickens because an untreated person with BPD also sees their partner as different people during splitting. The Borderline’s lack of perceptual integration keeps unsuspecting partners swinging on a pendulum between good and bad, and the “best” partner is eventually replaced by the “worst” partner. In either direction, their partner is damned if they do and damned if they don’t. Triangulation adds another dimension of perplexity because partners of Borderlines feel like they’re vicariously experiencing another relationship, albeit negative, with whomever is being triangulated against. According to ontological calculations, exactly how many people are involved in this tango has yet to be determined.
Oddly enough, people with BPD feel as if they’re always trying to please their partners, yet their partners will attest that they’re always trying to please their disordered companion. If the phrase “irreconcilable differences” applies anywhere, it would be here. To be fair, people with BPD will go to great lengths to maintain the appearance, itinerary, and feel-good sensations of a romantic relationship, but the mechanics that matter most for healthy relationships are missing, especially after the honeymoon period is forced to seek sobriety. Unfortunately, actuarial services for these types of relationships are often sold separately in family, civil, and divorce court (with occasional assistance from the police department). Peaceful breakups where everyone goes their separate ways ain’t gonna happen on the BPD tarmac. Former partners of Borderlines commonly report never being more smitten with and terrified by another human being, and they’ll often talk endlessly about the exhausting efforts they took to make things work. How could someone who felt so close become a complete stranger? How could someone who was given so much love and attention behave so horrifically? How could the most charming person I’ve ever met become the most dangerous? How could someone I cared about engage in the most cruel acts of revenge against me? How could this person believe, regardless of our differences, that I was against them? What more could I have done? The cognitive dissonance, incredulity, and paralyzing fear after such encounters frequently resume without cadence. Statistically speaking, traumatization and prolonged grief are the final products of these alliances. The psychological impact is incomparable, no matter how much time is spent trying to make comparisons. For a percentage of partners, the epilogue is nothing less than ruination and long-lasting rumination. Withdrawal and recovery from trauma bonds are undoubtedly some of the most emotionally difficult experiences known to humanity—akin to exiting a cult. Perhaps the spookiest aspect of Borderline Personality Disorder is that the disordered individual doesn’t understand how they’re affecting others; wouldn’t believe it if you told them, and believe that their behaviors are entirely justified according to their distorted perceptions and feelings. The shape of these relationships is chaotically circular, and the “shared” fantasy that draws partners in has absolutely nothing to do with equitable sharing among differentiated adults— it’s an illusory bond based on severe dependency. No matter how loving, patient, attentive, or forgiving their partner is, it’s ultimately up to the person with the disorder to decide whether or not the circle will be unbroken. And, to be sure, disordered people are not very good at making healthy decisions. For a person with BPD to admit defeat goes against their brutally conditioned survival instincts, even if it means they’re defeating themselves. When the dysregulated dust finally settles, Borderlines are damaged people who damage others as a consequence of their pervading instability.
A common complaint among partners of Borderlines is that they’re not the person they’ve been made out to be in the relationship, especially when splitting occurs. While this is certainly true on a fundamental level, and even more true based on the absurdly delusional bifurcation produced by splitting, partners of Borderlines often forget how much they’ve been altered based on their susceptibility to projective identification; how they’ve responded during conflict; what values they’ve jettisoned to make the relationship “work,” and their continued commitment to fulfilling various demands against their better judgment. In a sense, they’re setting themselves up to be split by contributing to the Borderline’s regressive rendezvous with repetition compulsion and disproportionate anger whenever it falters, albeit unintentionally. A more realistic observation would be to identify how much each partner has sacrificed of themselves to soothe the persistent anxieties of their suffering companion for a hopeful return of “the good stuff.” When this assessment is complete, they’ll undoubtedly recognize their inner contortionist and the contradictions they’ve entertained against their integrity. Along the compelling curve of codependent behavior, Borderlines are not the only ones who can suffer from a lack of positive self-regard. The continued pursuit of or long-term engagement with emotionally unavailable people often stems from unresolved childhood wounds of a similar nature that the partner of a person with BPD isn’t fully aware of. Any willingness to enable toxic traits requires admitting the role of an enabler while examining why certain traits are seen as attractive. Generally speaking, the amount of special attention required by untreated Borderlines is incomprehensible, no matter how capable or resourceful their partner believes themselves to be. Love, no matter who their lover is, will not cure an untreated Borderline. To thine own self be true begins with identifying what is or isn’t your true self and how to look out for its best interest rather than the obsessive interests of those who don’t even understand themselves. As for the person suffering from BPD, they’re not intrinsically or morally responsible for thoughts, feelings, or needs that originate from a serious mental health condition, but they must be held accountable for the negative effects of their neediness and the most consequential outcomes of their behavior; otherwise, their disorder will persist with impunity.
Overall, there must be a distinction between codependence as a toxic predisposition and codependency as an emergent behavioral dynamic that occurs during the process of communication and negotiation with a person suffering from Borderline Personality Disorder, or any other personality disorder (rigidity of character obstructs negotiation and relational equanimity). In other words, most partners of Borderlines are gradually converted into a state of situational codependency through recurrent interactions that become increasingly untenable. Just as there are people who possess borderline traits but do not meet full criteria for the disorder, there are also people who exhibit codependent traits (empathic sensitivity, conflict avoidance, and self-sacrifice) without being considered lifetime codependents (people with low self-esteem who seek approval and acceptance with an exaggerated sense of responsibility for the actions of others). However, a person who continues having relationships with pathological individuals may meet criteria for Dependent Personality Disorder. It should be recognized that Borderlines also share traits of Dependent Personality Disorder because of their core insecurities and emotional dependency. For this reason, they’re also vulnerable to being taken advantage of in abusive relationships—especially with narcissistic or psychopathic partners. Having BPD doesn’t mean that someone can’t have legitimate grievances or that their feelings are always driven by disorganized thought processes. Nonetheless, assertions made by a person with this disorder usually require an objective third party to separate emotional convictions from the evidence. Any behavior that occurs in relation to others should be evaluated on a spectrum, but codependent behavior of any flavor can quickly become a complimentary pathology when interacting with Borderlines. That being said, adult children of a personality disordered parent are far more likely to become subconsciously attracted to and enmeshed with someone suffering from Borderline Personality Disorder. Both partners in these relationships are symbolically returning to the womb for emotional nourishment that was unavailable during childhood. In these cases, codependence is “predestined” and likely pervasive in other contexts because of insecure attachment styles, set in motion by the reactivated resonance of archaic wounds. According to research, people who are exposed to conflict between their parents are more likely to demonstrate codependent behavior as adults, thinking of healthy relationships as boring and unfulfilling. In such cases, interpersonal chaos is seen as an exciting opportunity to fix something that could not be ameliorated in a former context. Echoes from the past reverberate until they crash into the present during a symbolic homecoming, as the brain tries to digest its formative leftovers in mysterious ways. To repair and reconcile parental relationships gone wrong is an unconscious impetus for many pathogenic alliances in adulthood. Historical familiarity is the most consequential vulnerability for individuals who come from generational trauma. Trauma bonds do not make good investment bonds because generational trauma is an equal-opportunity destroyer.
Perhaps Woody Allen summed it up best during his epilogue in Annie Hall: “It reminds me of that old joke, you know, a guy walks into a psychiatrist’s office and says, hey doc, my brother’s crazy! He thinks he’s a chicken. Then the doc says, why don’t you turn him in? Then the guy says, I would but I need the eggs. I guess that’s how I feel about relationships. They’re totally crazy, irrational, and absurd, but we keep going through it because we need the eggs.”
Borderlines presume that they will be abandoned, and then act in a manner that makes such abandonment virtually certain. — JBP
What’s interesting about Borderline Personality Disorder is that it represents a subset of pathologies that can upend therapy as a result of trying to effectively respond to it. Very few disorders have the power to expose a caregiver’s gullibility and naïve optimism like Borderline Personality Disorder. Therapists must be very grounded in their personal lives to withstand the strenuous provocations involved with BPD psychodynamics. Those suffering from Cluster B disorders unconsciously exploit the compassion of others because they’re starving for special recognition. BPDs, in particular, are subsisting in unimaginable emotional pain. As with all Borderline relationships, there are only three options for therapists to consider: Avoid, challenge, or appease. For any progress to occur, these clients need be challenged rather than appeased. However, BPDs don’t like being challenged because introspection and change is seen as evidence of their imperfections. Nonetheless, the power of love is only powerful if the person with the disorder can learn to love themselves while acknowledging the limitations and imperfections of others. It’s not that Borderlines are irredeemably “bad” people or fundamentally unworthy of love; rather, they’re completely baffled by the give-and-take dynamics required for healthy relationships. Borderlines confuse their inner experiences with the outer world until the two inevitably collide. Assuming that everyone will abandon them, there’s no room for negotiation or compromise. Borderlines are running scared, and this is why they repeatedly scare others away. To be clear, people with BPD would benefit immensely from stable companionship, but they must first develop the skills that allow for individuation, fear reduction, anger management, self-acceptance, self-compassion, and self-regulation. Therein lies the Borderline paradox: Part of the solution to a Borderline’s suffering is the availability of a stable relationship, but part of the reason why this disorder persists is because of how the sufferer behaves in relationships. Even if a Borderline found their perfect “soulmate” or object of blame, they’d still have all of their work ahead of them. As a disorder, BPD has characteristics that allow it to be proficient at obtaining relationships, but it doesn’t have the maturity or interpersonal skills to sustain relationships. Granted, relationships aren’t easy for anyone. Borderlines split in relationships in the same way that therapists split regarding their opinions about those suffering from this counterintuitive, misunderstood, and notoriously stigmatized disorder (the stigma is often related to the amount of pain and damage BPD causes for everyone). At the end of the dysregulated day, Borderlines need to learn how to have a healthy relationship with themselves. Nonetheless, silver linings must exist for both the patient and the therapist if meaningful insights are to be realized after such emotionally charged imbroglios. In retrospect, the message and value of compassion should not be determined by the origins or magnitude of our fragility.
We shall not cease from exploration, and the end of all our exploring will be to arrive where we started and know the place for the first time. — T.S. Eliot
In summation, the therapist was flummoxed by the patient’s misdiagnosis, victim identity, false self, emotional reasoning, dependency needs, and incomparable powers of projective identification when the therapeutic relationship was in its infancy. An underestimation of the Borderline’s internal disturbance resulted in normalizing what was clearly pathological. An erroneous confirmation bias was tenaciously defended, and the therapist allowed their own emotions to undermine the protective protocols of professionalism with an emotionally unstable patient. Instead of detaching, observing, and containing, the therapist has absorbed, deferred, and enabled—thereby becoming an enmeshed participant and all-gratifying object in the patient’s internal fantasy structure. Subsequently, the therapist’s shield of reason was systematically broken down by the patient’s idealization, aggressive demands for nurturing, distressed need for regulation, and intense fear of abandonment. What was easily recognized in the Borderline’s family of origin went unrecognized in the patient until it was too late. Something that should have been ruled out was regrettably overlooked and the therapist-patient relationship has taken its tragic toll. The appeasement to this type of mindset was preconditioned by the therapist’s upbringing (primed for propitiation) as provoked through coerced caretaking. This uncanny familiarity comes from a complicated dance that was set in motion many years before the clinician and patient finally met on that fateful therapeutic stage.
“The therapist’s perception of the patient as a victim—a perception that may be entirely valid with reality—results in specific forms of therapeutic zeal that may ultimately be counterproductive. In many cases therapists are characterologically predisposed to rescue fantasies because of childhood constellations involving a depressed mother or father and a long-standing pattern of playing the role of therapist in the family. Hence, the rescuer role, evoked through projective identification by the patient’s self-presentation as a victim, may attach to the therapist’s preexisting internal need to be a rescuer, and the two elements may function synergistically to produce formidable countertransference enactments,” according to Dr. Glen Gabbard.
Life can only be understood backwards; but it must be lived forwards. — Kierkegaard
Exploring adverse childhood experiences to understand how past relationships and unresolved conflicts have conditioned us in adulthood is what matters in the end. Memories, unconscious motivations, fears, desires, and embedded responses from interacting with our families of origin are reactivated for all participants during every therapy session. Many therapists are unable to identify the innumerable faces of transference or manage complex countertransference reactions whenever they emerge. Likewise, most patients are equally unaware of the influential depth that these symbolic-based forms of communication have on their own psychological motivations. Countertransference is the Achilles heel for therapists who become too invested in establishing meaningful relationships with their patients. Therapists who work with Borderlines must spend as much time developing and protecting their intrapsychic boundaries as they do protecting their external boundaries. A good question for therapists to consider is why they chose to work in the profession of caregiving to being with. For many, it could be related to the power of human connection; the virtue of compassion; the alleviation of suffering, and not wanting others to feel alone in their experiences. Most would agree that these values embody the essence of effective altruism. But can such aspirations become problematic? Are there exceptions to unconditional acceptance? Trying to lift certain people up in life without limits may result in them dragging you down (misery loves company), and this is an important lesson for all caregivers to learn. A Borderline patient will vigorously push for commiseration, comfort, and validation to avoid the painful process of rehabilitation, but providing too much of the former detrimentally postpones the necessity of the latter. Some mental health patients require impossible standards of care that can only be assuaged by learning how to love and care for themselves. A therapist should never abandon their professional identity to alleviate a Borderline’s fear of abandonment. As a final caveat, be careful what you care about.
There are two tragedies in life. One is to lose your heart’s desire. The other is to gain it. — George Bernard Shaw
Borderline Personality Disorder is perhaps the greatest paradox in the analects of human psychology. It’s a disorder that craves love, but it doesn’t understand the meaning of mature love. It’s a disorder that seeks relationships, but it doesn’t grasp the dynamics and limits of healthy relationships. It’s a disorder that yearns for proximity, but it doesn’t trust the sincerity of anyone who gets too close. It’s a disorder that begs others to experience its suffering, but it cannot see that this is the very reason why it continues to suffer. It’s a disorder that desperately seeks liberation from the outside, but it doesn’t realize that transformation comes from within. It’s an existential insecurity that cannot believe in the power of accepting itself, because it was not accepted when it began. It’s an anachronism searching for an idealized form of attachment. It’s desire without a solution and loneliness without resolution. It’s pain and terror cloaked in a bouquet of artificial flowers.
And your long-time curse hurts, but what’s worse
Is this pain in here
I can’t stay in here
Ain’t it clear?
That I just don’t fit
Yes, I believe it’s time for us to quit. — Bob Dylan
Stacking a house of unstable cards is naturally going to collapse if you don’t understand the true nature of what you’re stacked up against. Therapists who prematurely fold their boundaries in the face of a patient they don’t yet understand will lose the game every time. Betting against a Borderline’s nature is impossible, because they can always read the hand of accommodation you’re holding. Even when the mysteries of chaos are finally revealed, the embers from that raging Queen of Hearts will continue to burn.
This should have been a noble creature:
A goodly frame of glorious elements,
Had they been wisely mingled; as it is,
It is an awful chaos—light and darkness,
And mind and dust, and passions and pure thoughts,
Mix’d, and contending without end or order,
All dormant or destructive. — Lord Byron
In memory of John G. Gunderson (1942 – 2019)
For more information:
Click to access 15199_book_item_15199.pdf
Borderline Personality Disorder
Click to access 4Linda%20Baird,%20Childhood%20Trauma2.pdf
https://digitalcommons.pcom.edu/cgi/viewcontent.cgi?article=1064&context=psychology_dissertations
https://pubmed.ncbi.nlm.nih.gov/19461395/
https://forums.studentdoctor.net/threads/borderline-personality-d-o-and-countertransference.669569/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3342993/
https://mzwnylaw.com/psychology-today-borderline-personality-and-custody.html
https://www.psychologytoday.com/us/blog/toxic-relationships/201909/the-drama-loving-borderline
https://pubmed.ncbi.nlm.nih.gov/3966590/
Relationships and Borderline Personality Disorder
https://www.verywellmind.com/bpd-and-misdiagnosis-425176
https://www.bpdfamily.com/content/how-borderline-relationship-evolves
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1857277/
https://www.ncbi.nlm.nih.gov/pubmed/6846667
https://psychcentral.com/lib/loving-someone-with-borderline-personality-disorder/
Things which people suffering from Borderline Personality Disorder may do.
FAMILY GUIDELINES
http://www.bpdcentral.com/blog/?Fear-Obligation-and-Guilt-FOG-in-High-Conflict-Relationships-36
https://www.whatiscodependency.com/bpd-borderline-personality/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3330531/
https://mental-health-matters.com/borderline-personality-and-abuse/
How Personality Disorders Drive Family Court Litigation
https://www.ncbi.nlm.nih.gov/pubmed/8633685
https://www.sciencedirect.com/science/article/pii/S2352250X20301111
Click to access cp01604024.pdf
https://psychotherapy.psychiatryonline.org/doi/pdf/10.1176/appi.psychotherapy.2015.69.3.331
https://academicworks.cuny.edu/gc_etds/851/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9806505/
When Helping Hurts – How Professionals Become Negative Advocates – Or Not
Click to access Beth-High-Conflict-Family-Law-Matters.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3071095/
https://www.psychiatrictimes.com/view/breaking-hard-do-terminating-therapy-things-get-out-hand
https://expertpages.com/news/litigation_forum_acting_out.htm
http://www.continuingedcourses.net/active/courses/course093.php
https://www.zurinstitute.com/clinical-updates/borderline-one-away-from-losing-your-license/
https://nationalpsychologist.com/2014/01/psychodynamic-dangers-in-treating-bpd/102401.html
Recommended reading:
There is no doubt that healthy-mindedness is inadequate as a philosophical doctrine, because the evil facts which it positively refuses to account for are a genuine portion of reality; and they may after all be the best key to life’s significance, and possibly the only openers of our eyes to the deepest levels of truth. ― William James
The Sleep of Reason Produces Monsters is a phantasmal etching produced in 1799 by the Spanish painter Francisco Goya that depicts the imagined artist slumped over his desk, in a posture of nihilistic defeat, as ominous owls of madness and shadowy bats fly erratically overhead. This was Goya’s artistic commentary on Spanish society that he interpreted as succumbing to a lunatic’s brew of unmitigated fear, social antipathy, unrivaled corruption, and the liabilities of political unreason. The haunting image would persist as a representation of chaos whenever, as the poet W. H. Auden reminded us, the values of the enlightenment are driven away.
A little over two centuries later, in America’s post-fact zeitgeist of partisan sensationalism and multimedia gossip, the emergence of a toxic brand of emotionally volatile, identity-imbued populism threatens to destabilize society by appealing to authoritarian panaceas in the wake of geopolitical uncertainties. Relinquishing the faculties of reason, objectivity, dignity, and civil ethics when offered specious solutions for security or prosperity is as irresponsible as it is pernicious. After all, “total solutions” of Manichean simplicity are never realistic or sustainable in a world of increasing complexity and irreversible diversity. Just as Freud exposed the mind’s obsessive desire for a paternal caregiver during periods of crisis or vulnerability, we witness other parallels of uncritical yearning when people seek the mana-personality from Jung’s description of the collective unconscious. To mistake narcissism for competence is to mistake stentorian bravado for guidance. Likewise, to assume that personal significance or the assurance of safety can only be achieved through divisiveness is to perpetually recreate the very atmosphere of tyranny that one wishes to escape.
It appears that a grave deficit of cognition exists in the populace’s mind that prefers herd instinct to the arduous pursuits of objective analysis, social justice, moral philosophy, civil discourse, and scientific literacy. This belligerent lack of compassion, crude mockery of applied intellect, degradation of scientific methodology, and a selfish unwillingness to concede heterogeneity among communities has resulted in an abeyance of decency under the guise of exceptionalism.
Ideologies replete with paranoia, conspiracy, and mistrust were central to the atrocities of the twentieth century when varieties of fascism compensated for national insecurity. Balkanization was both anthropological and geographic in nature. As a result, mass trepidation created an isolationist vacuum for opportunistic absolutists to emerge. And their insatiable need for adulation would come at the endangerment of civilization.
As Thomas Hardy recognized, “If a way to the better there be, it lies in taking a full look at the worst.” Indeed. The evolved predicament of our human condition demands an identification of suffering; vigilant protection of social liberties; the maintenance of empathy; and an intrepid guard against the dangers of despotism if there’s any hope of achieving the means to an auspicious end. Otherwise, there will be no monster left behind.
Disclaimer: This essay is not intended to characterize all mothers suffering from Borderline Personality Disorder (BPD), nor does it suggest that Borderline mothers are inherently responsible for having mental illness. In addition, the following material is not meant to discount the positive outcomes or life lessons that can sometimes occur as a result of being raised by a BPD mother. However, it must be emphasized that Borderline Personality Disorder, also known as Emotionally Unstable Personality Disorder, is considered one of the most serious and complex mental health conditions in clinical psychology. Like most disorders, considerations should be taken to evaluate levels of functioning and severity on a full spectrum to avoid over-pathologizing or underestimating the psychological disturbance of the sufferer. Unless BPD mothers are in treatment; willing to seek specialized treatment; or willing to admit there’s a problem, they’re not going to be aware that they have a disorder—it’s up to their children, partners, and extended family members to develop this awareness. Generally speaking, BPD mothers are exceptionally resistant to being confronted or challenged, and they will invariably refuse to see themselves as disordered. From their perspective, being disordered implies being defective, “bad,” inadequate, or less than perfect. As long as the mother maintains control of her environment, while hiding behind a fortress of denial, there will be no incentive for cultivating self-awareness or embracing the process of change and potential recovery. Because of her resistance towards self-reflection, she will dismiss, minimize, or rationalize her behavior (deflecting and projecting rather than accepting). In essence, a BPD mother is a psychologically damaged parent “doing her best.” The problematic thoughts and behaviors of a person with Borderline Personality Disorder are not deliberate; they’re automatic. A BPD mother “means well,” according to her distorted perceptions, but she is not well. What needs to be understood are the devastating effects that Borderline mothers can have on their children’s emotional development, mental health, physical health, relationships, and ability to successfully achieve autonomy in adulthood.
No one chooses to suffer from mental illness, and no one chooses their parents. Likewise, no child can be held responsible for their parent’s emotional well-being, they can only offer compassion and work to discover themselves through the filter of time with the courage of honest reflection. To be clear, Borderline Personality Disorder is not a premeditated way of being; it’s a psychological predicament. Furthermore, this information is not designed to exculpate adult children of BPD mothers from their own contributions to unsatisfactory life outcomes, but it may offer clarity as to how their behaviors and ways of thinking were formed, influenced, and reinforced in toxic family environments. Borderline mothers don’t know how to interact in relationships, and a relationship with their children is just another type of relationship. Sadly, parental analysis and family of origin issues are generally the last frontiers of discovery for adult children of BPD mothers (children instinctively shy away from objective assessments of their parents out of respect, fear, or because they may feel like a traitor within the family system). Because Borderline Personality Disorder stems from a combination of neurobiological predispositions (genetics) and maladaptive survival mechanisms that were developed to cope with childhood trauma, it’s a condition that’s not suitable for effective parenting or intimate relationships. It’s not about blame; it’s about understanding.
If it’s not one thing, it’s your mother. — Sigmund Freud
In a previous post entitled Chaos and Elucidation: The Borderline Koan, I focused on the clinical challenges and professional liabilities that therapists may encounter when working with an undiagnosed or misdiagnosed patient suffering from Borderline Personality Disorder. More specifically, emphasis was placed on the preemptive identification of BPD in treatment settings, the Vulnerable BPD variety, and what to expect during emotionally charged clinical encounters. Here’s a quick review of the two-tier, conceptual classification system based on non-clinical observational impressions:
Authoritarian BPD Interpersonal disposition: Compulsively self-sufficient, domineering, mesmerizing, intrusive, anxious, irritable, worrisome, dysphoric, demanding, passionate, presumptive, judgmental, perfectionistic, fearful, competitive, impatient, pessimistic, combative, easily angered, petulant, stubborn, critical, paranoid, and envious. Attachment style: Fearful/Preoccupied. Intimacy style: Erotophobic (fearing engulfment more than craving intimacy). Rationale: “I have needs for stability, predictability, and approval that were not met during childhood; therefore, I must be in charge to survive.” Valence: Aggressive, flamboyant, anxious, intense, and irritable. Parenting style: Over-involved. Level of functioning: Moderate to high. Objective: Control of self-image, others, and their environment (overtly expressed).
Vulnerable BPD Interpersonal disposition: Dependent, charming, captivating, coercive, desperate, mercurial, seductive, playful, hapless, passionate, anxious, perfectionistic, dysphoric, duplicitous, suspicious, solipsistic, fearful, affectionate, labile, docile, angry, hypersensitive, desultory, fantasy-prone, childlike, vindictive, self-destructive, and jealous. Attachment style: Disorganized. Intimacy style: Erotophilic (craving intimacy more than fearing engulfment). Rationale: “I have needs for safety, validation, love, and nurturing that were not met during childhood; therefore, I must be taken care of to survive.” Valence: Coy, mischievous, needy, desperate, and enigmatic. Parenting style: Under-involved. Level of functioning: Low to moderate. Objective: Control of self-image, others, and their environment (covertly expressed).
For comparison, the Vulnerable BPD is similar to Theodore Millon’s Discouraged, Self-Destructive, and Impulsive subtypes, whereas the Authoritarian BPD strongly resembles the Petulant subtype. In relation to Christine Ann Lawson’s fairytale archetypes, Vulnerable BPD mothers would align with the “Hermit” and the “Waif,” whereas Authoritarian BPD mothers most closely resemble the “Queen” and the “Witch.” Of course, none of these categories are mutually exclusive, and there’s considerable overlap depending on environmental stressors, interpersonal variables, and social context. Ultimately, every character trait and behavior is on a continuum because BPD is a hybrid disorder that features significant comorbidity with mood disorders, behavioral disorders, and other personality disorders. Subclinical subtypes and colloquial descriptions, such as those incorporated in this essay, are convenient placeholders for purposes of conceptual taxonomy. Nonetheless, assessments of personality disorders in general should incorporate a dimensional model that emphasizes quantitative measurement.
Although Authoritarian BPD mothers can be highly functional and self-sufficient, they’re emotionally dependent. Conversely, Vulnerable BPD mothers tend to be both interpersonally dependent (poor self-efficacy) and emotionally dependent (poor self-regulation). Regardless of differences in presentation, relinquishing emotional dependency is the Borderline mother’s biggest fear because she would be forced to face herself, her past, her insecurities, her mental health challenges, and the comprehensive horror of her underlying pain and despair. In this sense, her fear of abandonment becomes an ancillary phobia, as it portends exposure of the mother’s deeply-rooted dependency issues. Authoritarian BPD mothers were usually parentified as children, whereas Vulnerable BPD mothers were often infantilized. When old enough to become parents themselves, this typology is reversed. In other words, the Authoritarian BPD mother will infantilize her children (mommy controls everything), and the Vulnerable BPD mother will parentify her children (mommy needs pampering). One mother strives to be seen as the “perfect caretaker,” and the other hopes to be “perfectly cared for.” The Authoritarian BPD mother compulsively seeks to do everything for her children, and the Vulnerable BPD mother wants her children to do everything for her. When the bell rings, Authoritarian BPD mothers walk into the ring swinging with a surplus of dominance, tension, and misplaced aggression. Vulnerable BPD mothers, on the other hand, are so fragile that they’re already lying on the floor and begging for assistance that will be used against the paramedics later on. Vulnerable BPD mothers are more likely to be viewed with opprobrium due to parental negligence, whereas Authoritarian BPD mothers are more likely to win Mother of the Year, as presented by a committee of uninformed bystanders, due to their excessive levels of involvement and compulsion for matriarchal supremacy. However, parental overinvolvement is also a form of neglect because it discourages a child’s individuality and invalidates their emotional experiences. Having what is considered an externalizing disorder (external locus of control), Borderline mothers search for external sources of stimulation, validation, and emotional regulation. They also search for external sources of blame to avoid feelings of humiliation and shame. Without the ontological grounding of interiority (a stable sense of self), life, in all of its splendor and terror, must be experienced by acquiring a continuous supply of outside reminders to reassure the Borderline mother that she exists.
In this essay, we’ll be examining the Authoritarian BPD mother (overinvolved and emotionally immature) from the perspective of motherhood; how this disorder affects the mother’s children during development, and the ramifications of long-term exposure caused by interacting with a mentally disordered parent. Authoritarian BPD mothers could be thought of as having an extreme “smothering” or “hovering” parental style (i.e., overprotective, “devouring,” and overbearing) that interferes with their children’s potential for autonomy in the name of love. According to Freud, an Authoritarian BPD mother represents the oedipal mother. Theses types of BPD mothers represent the proverbial “helicopter” parent without a landing pad, and their ability to undermine the growth of their children is boundless. They also incorporate a fairy godmother fantasy defense to justify their need for dominance during family interactions, but the damsel in distress and princess in the tower motifs are also available for situational convenience.
People often say that “every family is dysfunctional,” but family of origin problems are disproportionately corrosive whenever children are raised by a Cluster B parent (narcissistic, anti-social, borderline, or histrionic). Children also learn about love and relationships from watching and interacting with their primary caregivers. Virtually every relational interaction that transpires, including the relationship we have with ourselves, is conditioned by our parents during childhood. Most children of Borderline mothers have learned to normalize the abnormal, because the abnormal is all they’ve ever known. Likewise, BPD mothers have unconsciously normalized the abnormal due to their own traumatic childhood experiences. However, mental illness among primary caregivers is not the same as mental illness among siblings and relatives. Proper emotional attunement with one’s biological mother is, arguably, the most influential factor for developmental congruency, self-actualization, and independent success in adulthood. Regrettably, Borderline Personality Disorder is a disorder of the self.
Some of the most common traits of Borderline mothers include the following:
As noted in the classification section, there exists two basic parenting styles among Borderline mothers: Overinvolved and under-involved. But these polarized approaches to parenting can temporarily switch according to various changes in the Borderline mother’s mood while exacerbated by splitting and passive-aggressive behavior. For both Vulnerable and Authoritarian BPD mothers, an inability to regulate conflicting emotions during stressful interactions creates havoc for other family members as they try to interpret and effectively respond to such perplexing, contradictory, and unpredictable dynamics. Borderline mothers are infamously known for being erratic, dramatic, and emotionally volatile. BPD mothers are also known for choosing either narcissistic or passive/codependent partners, but many end up living alone because of recurring marital, romantic, and interpersonal conflict. BPD mothers are intense and exert a persuasive hold on their children’s feelings (emotional incest). This dynamic occurs when a child feels responsible for attending to their mother’s emotional well-being; it also occurs when the mother cannot get her emotional needs met by her spouse or other adults. In tandem, the mother’s children will feel obligated to predict, interpret, and appropriately respond to their mother’s conflicting feelings, thoughts, and needs.
What’s all of this “need” about? The French psychoanalyst Jacques Lacan emphasized the concept of “lack” as a powerful motivation for human behavior. And, to be sure, the Borderline mother is lacking in crucial developmental features due to various forms of childhood deprivation that produce cognitive deficits affecting her emotions and ability to relate to self or others (object relations). In essence, the Borderline mother’s developmental deficits from a bygone era transmogrify into relational deficits that adversely affect her interactions with others. To compensate for these deficits (missing internal regulatory mechanisms), she desperately seeks someone who is willing to provide a simulacrum of these ingredients (essential ego functions) so that she can feel whole and secure. By latching onto someone, her unconscious hope is that they will become a stable, safe, and soothing introject. The problem is that her brain’s way of healing itself is by obtaining exogenous (external) remedies for endogenous (internal) deficiencies instead of facing her fears and committing to the psychologically painful work necessary to acquire introspection and emotional self-sufficiency. In other words, the Borderline mother outsources her regulatory needs to offset instability with the additional hope of fulfilling archaic loose ends from a childhood gone awry. In essence, the mother is motivated by her deficiencies and her longings are expressed in a unique array of maladaptive behaviors. Furthermore, alterity (individuation) makes her nervous because it provokes separation insecurity, which makes her feel abandoned and unsafe. Her identity is diffuse because her core is empty, so she becomes a huntress on an insatiable mission to fill the void. As a consequence, the person (aka “favorite person” or intimate other) she unconsciously “uses” to achieve course correction either implodes under the weight of her endless needs or they withdraw because they finally realize the importance of their own survival. Without being able to objectively evaluate her thoughts, feelings, and behavior, the Borderline mother is oblivious to the insidious effects her actions have on others. Overall, her most cherished supporters become collateral damage in the wake of her neediness, anxiety, panic, paranoia, and anger. To psychologically fuse with a partner, spouse, or child is a life-or-death imperative for the BPD mother, but it eventually results in the paralysis of potential for all participants in her path. Borderline mothers do not intend to behave as they do, but they do intend to get their needs met by all means necessary. Whenever denied, frustration is converted into aggression as a method to achieve control. Consequently, the Borderline mother cannot relate to her children as they are; she can only identify with them to the extent that they’re capable of serving the exigencies of her residual deficits. As if all of this wasn’t daunting enough, the Borderline mother’s lack of object constancy signifies that she will expect frequent contact to temporarily assuage her inner turmoil.
Borderlines have an uncanny ability to notice specific details about other people, but they lack insight when it comes to their own behaviors or how others perceive them (an understanding of the impact they have on others is conspicuously absent from the Cluster B modus operandi). It cannot be emphasized enough that people with BPD know only too well how other people are affecting their emotions, but they cannot comprehend how their behavior affects others. The Borderline’s interpersonal awareness is vigilant, but it’s filtered through a distorted lens of mistrust, beset by frequent misinterpretations regarding the intentions of others. BPD mothers can ostensibly recognize the hardships of their children, but they cannot authentically connect because of their own anxious preoccupations and compromised theory of mind. In addition, Borderline mothers compulsively seek advice due to impaired reality testing while simultaneously defaulting towards their own brand of maladaptive self-determination. A Borderline mother’s capacity for empathy, although high in emotional sensitivity, is self-oriented, and she experiences exceptional difficulty with cognitive empathy (empathic accuracy). Whenever her immediate needs are frustrated, consideration for others is often the first thing that goes out the window. Simply put, she cannot understand the perspective of others, especially in the heat of her most current crisis. An inability to see other people as stable and integrated human beings (whole object relations) is paramount to understanding the Borderline mindset. It’s the mindset of trauma, and trauma cannot get outside of itself. Deficits in mentalization (reflective functioning) interfere with the Borderline mother’s ability to accurately perceive other people or to form realistic impressions. As a result, there’s a significant gap when it comes to understanding the emotions, thoughts, and intentions of others. Unable to integrate positive and negative aspects of herself, she’s unable to do so with others, thus dichotomizing people into gratifying or frustrating objects (“good” or “bad”). Such rigid evaluations are bereft of nuance and complexity, hence she is always interacting with a “distorted other,” which aggravates her apprehension. The Borderline mother is afraid of the individualism, maturity, and agency of those around her because autonomy represents unpredictability. Consequently, fear becomes her GPS because she may not be able to control what others think about her or what they might do in her presence (i.e., disappoint, reject, hurt, humiliate, or take advantage of her). She is dubious and always testing the waters. Her way of coping with potential “stranger danger” is to either push people away or pull them into her narrow psychological jurisdiction.
For her children, the mother’s attempts to relate may feel superficial or insincere because people with BPD have problems with differentiated relatedness. Borderlines can often identify the emotional states of others via mental state discrimination, but they have difficulty interpreting them in a non-personal way due to self-referential hypersensitivity, which includes paranoia and catastrophizing. BPD solipsism will ultimately override any concern for the needs, challenges, and limitations of others. In reality, the Borderline mother feels engulfed by the emotional needs of others because her own are insurmountable. Internally mismanaged by a combination of insufficient mentalization and alexithymia, she cannot understand the intense nature of her own emotions, let alone comprehend the complex emotional experiences of her children. Emotionally speaking, the Borderline mother cannot stand on her own two feet. As a consequence, her children become representational objects who are expected to support their mother’s unending psychosocial dilemmas. In a fundamental sense, the children of a Borderline mother are instrumentalized to serve her needs. Minimizing ambiguity reduces fear, so it’s easier for the mother to invalidate her children’s emotional experiences and personal struggles rather than being overwhelmed by their complexity. She is, after all, consistently overwhelmed by her own emotions (aka the “dead mother” complex) and was invalidated herself while growing up. The mother’s priority is, paradoxically, to rely on her children for stability, security, reassurance, validation, and emotional comfort. As a result, her children become involuntary enablers via psychological fusion during a codependent process of incremental enmeshment. In other words, the children unwittingly fulfill important psychological functions for their mother by becoming her external regulators, crisis attendants, guardians, and “redeemers.” Overall, they become their mother’s recharging station to generate feelings of safety, self-esteem, and selfhood that she cannot endogenously produce for herself. Despite the crucial role her children play as representational objects, they also become objects of frustration because they remind the mother of her own childhood, fears, developmental lacunas, and innate vulnerabilities.
Along the contours of the Karpman drama triangle, the BPD mother (self-identified victim) has a tabloid-worthy issue with something or someone (persecutor), and her children (rescuers) are implicitly or explicitly expected to support her grievances while making intrepid efforts to “fix” her problems. She comes across like a bewildered and agitated project manager who insists that others agree with her blueprint of never-ending complications and commit to doing her bidding according to her shifting expectations. Sadly, these problems are seldom resolved in a way that’s considered satisfactory to the mother; ergo, the victim-persecutor-rescuer cycle continues or intensifies as new complications emerge (having a persecutory object justifies continued dependency, and a great deal of time is spent chasing imaginary demons). Throughout this dynamic, the children begin to identify as crisis attendants while their mother resolutely identifies with the drama of each crisis. The pressure to merge with the velocity of her emergencies is profuse. Slowly but surely, her children begin to feel confused, anxious, and inadequate about their ability to effectively manage future predicaments. While their confidence for handling these situations erodes, a theme of trepidation, incompetence, self-doubt, negativity, and failure will affect other endeavors as they grow older.
Regrettably, the image of motherhood is more important to BPD mothers than the mechanics of effective parenting. What reflects well on the mother is usually prioritized over what’s beneficial for the child. Since most Borderlines were raised in abusive and invalidating environments, they’re unable to give to their children what they never received. People with BPD typically experienced life in a chaotic household with emotionally negligent, disruptive, or physically abusive parents who also suffered from personality disorders or other forms of mental illness. Subsequently, the survival mechanisms that the helpless little girl developed to cope with childhood trauma are reflexively incorporated into maladaptive ways of thinking and behaving whenever she leaves home to establish her own family. These primitive defense mechanisms may have been useful for protecting a traumatized and hypersensitive child, but they invariably outlive their usefulness in adulthood. Regardless of its immediate survival value, fear conditioning does not bode well for optimizing human flourishing over time. The Borderline’s fight-or-flight response never turns off because they’re forever fractured by trauma and operating in self-preservation mode. Ironically, the BPD mother recreates in her nuclear family the very toxic conditions that she tried to escape from when she was a child. She may also try to establish the “perfect” domestic atmosphere of her imagination that often feels restrained, eerie, forced, and artificial. In essence, the psychological pain that she cannot face from her past reanimates itself in the present as she attempts to gain mastery over unresolved conflicts. Subsequently, the trauma bond that the mother experienced with her parents is reestablished with her children as they become unwitting participants in a theatrical revival by receiving a bootleg version of their mother’s upbringing (it’s an experiential palindrome that resembles phantom limb syndrome; the original source of pain has subsided but the residual damage is recycled in the present). Since her most abusive parent maintained power within the family unit, the Borderline mother learned to covet the bully. She also craved love and attention from a parent or parents whom she feared (disorganized attachment). Because love and fear cannot exist in the same space, she disappeared into the fragmented wasteland of structural dissociation. This pathological system of tragic embodiment and traumatic interrelatedness continues because the BPD mother personally identifies with abuse, instability, victimization, and impending doom (most borderlines were victims of narcissistic abuse who later become unconscious purveyors of narcissistic abuse). In other words, she checked out a long time ago and her body is on autopilot. More succinctly, the mother who runs the home is not at home.
As Christine Ann Lawson stated in Understanding the Borderline Mother, “Chronic psychological degradation of a child, or an adult, can have deadly consequences.” Fear, paranoia, panic, impulsivity, confusion, irritability, anger, and a constant need for reassurance to avoid feelings of abandonment (severe separation anxiety) are the hallmarks of an anxious child who never developed a secure attachment to a reliable caregiver during the first few years of life. Accordingly, the BPD mother is living in a state of eternal recurrence with “the world is against me and it’s your job to recognize my suffering” mentality (unrelenting crisis). It’s the portrait of an insufferable sufferer. As the painting suggests, she’s the embodiment of emptiness and fear because she was neglected and rejected by her original caregivers. Furthermore, honest expression of feelings and self-exploration were either prohibited when she was growing up or seen as a weaknesses, so she maintains this repressive motif through a combination of dissociation and denial to avoid further feelings of shame. As she continues to grieve the loss of her youth without sufficient solace, she invites her children to share in the travails of her reverberating misfortune. Consequently, BPD mothers fear the prospect of meaningful change because change symbolizes the unpredictability of their childhood and reminds them of not being in control. Receiving mixed messages from abusive parents translated into assuming mixed messages from others, thus setting the stage for the mother’s paranoid ideation, approach-avoidance attachment style, passive-aggressive behavior, and repetition compulsion. There’s a war going on inside her head and no safe space can be found. The mother feels as if she’s always being acted upon, even when she’s acting out, and her survival will always be prioritized over slowing down enough to initiate honest self-analysis.
Borderline mothers often grew up in a state of extreme emotional deprivation, so they will spend the rest of their lives trying to compensate for developmental and attachment deficits. However, their method of obsessive-compulsive overcompensation (anankastia) causes lifelong relationship problems with just about everyone they get close to. To make matters worse, the Borderline mother unconsciously seeks psychological equilibrium at the expense of her children and significant others. Because unresolved trauma keeps the Borderline mother in a state of arrested development, she’s essentially a mommy who needs a mommy and a child trying to raise children of her own. The Authoritarian BPD mother, in particular, is overprotective to a fault because she’s symbolically protecting herself.
From the FOG website: I have been emotionally wounded and crippled by my early life experience, from which I have never healed. The pain and neurotic anxiety drive me to live vicariously through my children. I somehow believe that if I can keep them under my control, the scared little girl that lives within me will at last feel safe and protected. I am putting my emotional needs ahead of my children’s developmental needs, and on some level I know this. I can’t stop because I’m addicted to the soothing feeling of reassurance that having control provides.
Simply put, what happens in childhood does not stay in childhood.
Children of Borderline mothers are also at high risk for developing BPD, or some other personality disorder, due to strong hereditary and intergenerational influences. Others may try to model their mother’s behavior until they realize that it’s abnormal, unsustainable, ego-dystonic, and profoundly unhealthy. More often, children become collateral damage in the wake of their mother’s overwhelming desire for control and enmeshment, which results in succumbing to various mental health problems while spinning their wheels. As the child’s need for healthy exploration is stifled by their mother’s need for control, so is the child’s capacity for developing independence in adolescence and early adulthood as the umbilical cord becomes a leash. The emotional neglect, drama, and abuse that the mother endured during childhood is unconsciously reenacted in her intimate relationships and approaches to parenting (i.e., poor communication, feelings of victimization, interpersonal conflict, psychological projection, explosive anger, emotional reasoning, controlling behaviors, and disproportionate overreactions to perceived slights or threats). *Some BPD mothers experience transient psychosis or engage in suicidal behavior during periods of extreme emotional decompensation. Although the BPD mother may feel and fervently believe that she is nothing like her parents, she has unknowingly internalized faulty perceptions and behaviors from enduring adverse conditions during childhood. The chaos of the Borderline’s mindset is later projected onto their surroundings because they see the environment as a canvas to capture and reflect their inner suffering. In other words, “my pain must be painted everywhere to verify that my suffering is not in vain.” The mother’s feelings become facts (psychic equivalence), and she externalizes causation. It’s a theatrical cry for help, but meaningful assistance meant to elicit qualitative change and insight will undoubtedly be met with defiance because the source of her misery is always peripheral. Likewise, children of BPD mothers may subconsciously mirror and endorse their mother’s values, beliefs, behaviors, and attitudes through projective identification, which can result in exaggerated overidentification (many of the mother’s maladaptive coping skills for managing stress are inherited or modeled by her offspring). By introjecting their mother’s tension-infused and paranoid worldview, her children will receive validation and support, but they ultimately sacrifice their own sense of identity through the maintenance of an unhealthy alliance. Without developing a robust sense of independence, a pattern of codependency typically ensues, which includes low self-esteem, a strong need to please others (fawning response), feeling responsible for other people’s problems, and difficulty setting boundaries. Codependent behavior is linked to having parents who ignore their children’s needs, parents with narcissism or other personality disorders, controlling or overprotective parents, and parents who resort to bullying when challenged or frustrated. Conceptually speaking, the “speed of need” represents the BPD mother’s core dependency issues and the “speed to accede” captures her children’s propensity for codependency.
“Mothers with BPD tend to give feedback and validation to their children largely based on whether or not the child pleases the parent rather than objective feedback. They define the self-worth of the child based on the ability to please others and hence encourage them to build an identity around being a people pleaser. This is an unhealthy form of selflessness that compromises the child’s self-confidence,” states Daniel S. Lobel, Ph.D.
Trauma bonding (aka betrayal bond), a term coined by Dr. Patrick Carnes, occurs when a person experiencing physical or psychological abuse develops an unhealthy attachment to their abuser through intermittent positive reinforcement. Untreated people with BPD automatically lay the groundwork for contentious dynamics because they suffer from a relational disorder that demands too much accommodation from significant others. Without being able to respect the personal space of loved ones, mothers who suffer from this disorder will cause their children to suffer. Although unintentional, a BPD mother’s primary intention is to get her needs met, and this places an unsustainable burden on her children. The children may rationalize or defend abuse; feel the need to maintain loyalty; isolate from others, or hope that their abuser’s behavior will change. Because there’s always a payoff for staying bonded to a Borderline mother, occasional rewards (psychological or material) will discourage thoughts of “betrayal,” which is really nothing more than healthy maturation. Not allowing her children to separate, the Borderline mother hinders individuation and promulgates emotional incest during infancy, adolescence, and adulthood. Over time, the mother’s children become the equivalent of codependent zombies; sequacious, obsequious, and anxiously awaiting their next set of instructions (the Norman Bates effect). Disagreement with the values, feelings, and beliefs of a Borderline mother is not an option, and she will invariably get her way in the end.
The following are commonalities in parenting behaviors that typify mothers with Borderline Personality Disorder: (1) they use insensitive forms of communication; (2) are critical and intrusive; (3) use frightening comments and behavioral displays (Hobson et al., 2009); (4) demonstrate role confusion with offspring (Feldman et al., 1995); (5) inappropriately encourage offspring to adopt the parental role (Feldman et al., 1995); (6) put offspring in the role of “friend” or “confidant” (Feldman et al., 1995); (7) report high levels of distress as parents; (Macfie, Fitzpatrick, Rivas, & Cox, 2008); and (8) may turn abusive out of frustration and become despondent (Hobson et al., 2009; Stepp et al., 2012).
In a research article entitled The link between personality disorder and parenting behaviors: A systematic review: “The links between personality disorder, attachment insecurity and child maltreatment identified in the literature above goes some way to help explain the frequently observed intergenerational transmission of child maltreatment (Pears & Capaldi, 2001). Parents with personality disorder may be particularly vulnerable to treating their children in the same way that they themselves were treated. Indeed, Adshead (2003) claims that the children of personality disordered parents may be placed at risk of physical and emotional harm as a consequence of the emotional difficulties, dysregulated affect, hostility, unusual cognitions and preoccupation with the self that characterize aspects of personality disorder. Cordess (2003) more specifically asserts, that different personality disorder subtypes are likely to (negatively) impact on parenting in specific ways. In a review specifically relating to the children of mothers with Borderline Personality Disorder, Lamont (2006) identifies these children as disadvantaged and at high risk of future psychopathology as a direct consequence of their mothers’ borderline symptomatology.” To make matters worse, stress hormones, which are notably higher among Borderline mothers, are passed through the placenta to shape the brain and nervous system of their offspring, which causes their children to become even more susceptible to the interpersonal vagaries of their mother’s pathology after birth. Because mothers with BPD have difficulty coping with stress (low distress tolerance), their mere presence acts a chronic psychosocial stressor for their children.
15 signs of toxic parenting, as compiled by Dr. Sharon Martin, include the following:
Unfortunately, children and adult children of Borderline mothers often succumb to problems with low self-esteem, depression, anxiety, PTSD, compromised identity, addiction, age regression, hypervigilance, derealization, depersonalization, obsessive-compulsive behavior, addiction, escapism, defensive posturing, rebellion, rumination, emotional repression, sexual repression, confusion, apathy, procrastination, perfectionism, chronic fatigue, despair, negativity, stress-related illnesses, self-hatred, and suicidal ideation. *Many children and adolescents with noted behavioral problems are often reacting to the effects of living with a mentally ill parent or being raised in an invalidating/chaotic environment. Adult children of BPD mothers are also more susceptible to being involved with high-conflict or pathological relationships through programmed familiarity (operant conditioning via insecure attachments) that result in conflating love with trauma bonding, which unconsciously associates nurturing with abuse. Ultimately, compulsive attempts to assuage or win the approval of others becomes more important than believing in oneself. However, some adult children of BPD mothers resign themselves to permanent isolation due to chronic self-doubt, feelings of unworthiness, hopelessness, and recurring fears of inadequacy. A conspicuous lack of self-respect while distrusting one’s intuition outlines the child’s concept of self as they enter adulthood; perpetuated by a fatalistic belief system (internalized bad object). Other traits that emerge among children of Borderline mothers include excessive rumination, self-criticism, inhibition, and a negative (pessimistic) attributional style. Worst of all, children of BPD mothers often fail to achieve autonomy, which results in lifelong problems with insecurity and feeling as if they have been “left out” of the adult world. Ultimately, there’s a failure to launch, or a failure to launch correctly.
Since the BPD mother has a monopoly on Weltanschauung and a competitive need for supremacy, her children may grow up feeling helpless, guilty, or ashamed for trying to assert or express themselves. Because these children have learned to mistrust their intuitions, they’re usually convinced that the problem must be with them instead of their mother or the family system. Subsequently, the children often end up with the exact same mindset as their mother (i.e., feelings of unworthiness, fear, and insecurity) as they internalize a large arsenal of negative beliefs about themselves and others. For example, daughters of Borderline mothers frequently report feelings of shame and sons of Borderline mothers often report feelings of being emasculated. An overwhelming fear of vulnerability contaminates the children’s relational potential as safety and suppression are chosen over exploration. When mounting frustrations finally breach the levee, a flood of depression, anxiety, and despair inundate the children’s psychological landscape. If the children are lucky enough to escape the impact of family chaos by early adulthood, they may continue to live in a state of vicarious suppression and unconsciously deny themselves the freedom of psychological separation. Essentially, the mother’s emotional dysregulation fosters developmental dysregulation in her children, and her shame is sponsored by proxy. Inconsistencies in parenting are a force multiplier for creating inconsistencies in a child’s ability to acquire self-esteem or manage their own lives as they get older. Sometimes these delays in childhood development are overcome in adulthood through experiential contrast, therapy, healthy relationships, career involvement, and the establishment of adequate spatial and emotional distance from the BPD mother. More often, these children remain in the dark; become disillusioned; continue to suppress their emotions; experience low levels of confidence; embrace futility; resort to self-sabotage, and eventually wonder what in the hell went wrong.
The stress of parenting causes Borderline mothers to disregard healthy discipline that promotes growth, independence, and self-respect in favor of various forms of abuse that foster inhibition, confusion, shame, humiliation, insecurity, and fear (abuse that was normalized during the mother’s upbringing). However, BPD mothers don’t think of themselves as abusive, because their combative behavior is a natural byproduct of their disorder (misplaced aggression); besides, it’s all they’ve ever known (ego-syntonic rationalizations for ego-dystonic emotional states). In other words, all thoughts, feelings, and actions are self-justified. Psychological abuse through emotional neglect, verbal attacks, criticism, mocking, “smothering,” and/or physical abuse enacted by draconian methods of punishment are the methods of choice for BPD mothers when raising (aka controlling) their children (people with BPD gain an unusual amount of psychological satisfaction from enacting punishments via their adherence to the talionic impulse). In addition, the mother’s impulsivity, if not recognized in other behaviors, will typically manifest in her reflexive need for control, which rapidly impinges on the space of others. But whenever her children become adults, the mother’s need for control will likely manifest along surreptitious delivery systems (e.g., financial control, compelling ultimatums, “emergencies,” or unreasonable demands for attention and proximity that appear reasonable). In such cases, children may feel intimidated or annoyed by their mother’s intrusiveness and neediness while simultaneously feeling obligated to acquiesce for the sake of comity. Furthermore, children of the disordered frequently question their own sanity, as their mother assumes absolute authority concerning the nature of reality.
BPD mothers see their children as extensions of themselves, or much needed parts of the self (need-gratifying objects), to stabilize their emotions and provide a sense of identity. After all, the role of being a mother provides some degree of identity fulfillment. Unfortunately, the Borderline mother relies too much on her children for purposes of commiseration and reassurance, which turns the mother-child relationship into an indispensable support structure for a clinging parent. Her dependency needs are counterintuitive and often misunderstood because she exhibits unparalleled levels of hardheadedness, stamina, and determination. Furthermore, an Authoritarian BPD mother’s need for dominance creates an Animus possession (masculine tyrant persona) to ensure capitulation to her needs. What transpires is a BPD brand of pissed-off dependency, protected by a firewall of indefatigable irrationality. Love becomes a conditional possession for the BPD mother, but her children are repeatedly subjected to tests and confirmations to prove unconditional love for their mother, with the not-so-subtle implication that separation equals betrayal. Because of the mother’s unrivaled need for control to avoid feelings of abandonment, her children will invariably feel obligated to serve as their mother’s emotional wet nurse, surrogate partner, surrogate parent, best friend (aka favorite person), confidant, savior, apologist, negative advocate, object constancy regulator, blame container, safety provider, therapist, or consigliere. However, the enormous pressure placed on any child to fulfill such unrealistic and unsustainable roles will eventually result in a codependent relationship that’s emotionally exhausting, confusing, and disturbingly counterproductive. Subsequently, there will be nothing left when it comes to the children’s emotional needs and essential requirements for personal growth. The underlying message is that independence is a rejection of the mother and justification for her to criticize or reject the child. This dilemma places a great amount of obligational stress on the children to be available for their mother instead of themselves. Consequently, manufactured divisions among siblings may include the “hero child,” the “scapegoat child,” the “golden child,” and the “caretaker child.” These narrowly defined roles often become self-fulfilling prophecies in pathogenic families. Instead of having a broad range of independent qualities that contribute to and encourage the formation of a healthy family unit, the children become typecast members of a disorganized pedigree with low levels of family cohesion.
Borderline mothers employ a combination of fear, obligation, and guilt (FOG) to ensure that their children remain loyal and continually invested in their inconsolable emotional needs. However, the mother’s desperate search for stability, ironically, results in more instability. Because of the mother’s intolerance of being alone (autophobia), her children may feel compelled to rescue her from drowning in sadness, uncertainty, loneliness, and worry. Borderline mothers are caregivers who need caregivers, so their unmet needs remain counterintuitive. In many cases, her children provide an opportunity for the mother to establish a corrective relationship as compensation for a lifetime of insecure attachments. In fact, this is why BPD mothers often perceive their children’s friends or romantic partners as potential sources of competition who inconveniently take away from her need for attention, affection, resources, and dominance. In other circumstances, the mother may engage in inappropriate conversations or interactions with her children’s friends or come across like the mom who acts like a teenager. The ultimate desire to isolate her children from the influence of diverse socialization allows the BPD mother to feel in control of family commitments while avoiding feelings of separation insecurity (additional power is achieved through restrictive control of resources and outside activities). To maintain an in-group/out-group mentality solidifies an “us versus them” climate of fear that promotes mutual dependencies, ushered in by the mother’s black & white thinking. Ironically, the mother may even compete with her own children, or become visibly envious, as if they were rivals who must be subdued and defeated (narcissistic rivalry results in dysphoria when others succeed and elation when others fail). In some cases, her envy can become so virulent that it extends to being envious of her children’s accomplishments, material possessions, happiness, relationships, and stability.
Regarding overlapping traits of Narcissistic Personality Disorder (NPD), the BPD mother’s compensatory grandiosity is exposed through her sense of entitlement, interpretive infallibility, paranoia, psychic equivalence, and fantasies of omnipotence, especially during periods of emotional decompensation. Although BPD and NPD comorbidity is possible (some studies suggest up to 40%), an untreated Borderline mother is already the reification of “main character syndrome,” so extra solipsism need not apply. Her children must act as a mirror to reflect her inflated self-image while counterbalancing how deflated she really feels whenever the curtain is lifted. In this sense, narcissistic defenses protect against negative affectivity. To reduce the agony of her inner turmoil, she doubles down on her arsenal of passive-aggressive behaviors and outright viciousness. For example, to be the adjudicator of other people through binary assessments is profoundly narcissistic, regardless of the mental deficit that makes dichotomous thinking prevalent (poor object relations). Likewise, judging others based on how they affect one’s feelings during any given moment is the height of self-absorption. As noted in Chaos and Elucidation: “Ironically, some people with BPD will accuse anyone who isn’t focusing on them of narcissism, especially if there’s a diminution of appeasement from their favorite person.” The mother sees herself as sui generis, but her theatrical posturing and ostentatious declarations are imbued with crushing insecurity that fully reveals itself under stress. She prefers gossip when faced with the challenges of complex social interactions and resentment is always lurking in the shadows, enveloped by an ongoing persecution complex that provides her with a sense of meaning in the face of uncontrollable variables. To be the subject of persecution is to be special, and being special demands special consideration from others. For the most part, rejection sensitivity aggravates narcissistic and antisocial behavior in people with BPD, and the expression of these traits is generally contingent on the severity of emotional decompensation. Nonetheless, Borderline mothers continually compare themselves with others and unknowingly influence their children to doubt themselves by default. When the mother repeatedly compares her children’s upbringing with her own upbringing, or compares her success with her children’s success, this only demonstrates the persistence of her unresolved internal conflicts. Healthy parents do not compare themselves with their children, but Borderline mothers see life as a competition that they must win at all costs. Subsequently, the children’s need to believe in themselves is overshadowed by the belief that their existence is integral to their mother’s capricious emotional needs. Afraid of her children’s potential for autonomy, they do not have permission to thrive without her consent and authorization. Her children are her property, and she is reluctant to share her property. Of course, proprietary preoccupations represent another form of egocentricity. She sees her children’s growth and maturity as a sign of rejection and an existential threat to the fragility of her tenuous selfhood (separation equals mental obliteration). If something positive happens to the children, it must include the mother, or it must be facilitated by the mother’s oversight and approval (no differentiation without representation). Begrudging behavior typically follows her tendency to pass judgment, whether explicitly or implicitly. Due to poor social cognition, the Borderline mother does not see her bulldozer-driven compulsion for interference and conceited sense of entitlement as inappropriate. When it comes to aggressive intrusion, it’s important to remember that boundaries of all types are anathema in dysfunctional families. Again and again, the family’s attention returns to the center stage of BPD predominance—held together by the clinging weight of propinquity.
The mother’s tendency towards jealousy and suspicion can result in blatant disapproval of her children’s acquaintances or accomplishments to displace her own insecurities and fear of abandonment. Likewise, BPD mothers often triangulate family members by means of favoritism, scapegoating, gossip, the silent treatment, criticism, shaming, derogatory humor, and forced allegiances. The mother will frequently alternate between praise (idealization) and criticism (devaluation) of her children according to the athleticism of their attentiveness. If guilt is habitually weaponized by the mother, it usually manifests by letting her children know how unappreciative they are of the sacrifices that were made for them. However, it’s often the case that many of these “sacrifices” were not requested by the child nor implemented to ensure success independent from the mother’s motivations. More often, these gestures represent a means of manipulating the child’s emotions by making them feel indebted and shamefully dependent because, let’s face it, they’re ultimately undeserving of any act of generosity that was originally denied to their mother. On some level, the mother knows how much she sacrificed as a child to appease her caregivers, so she feels that her family is obligated to emphatically acknowledge whatever she does for them. In response, her children may start feeling like Pavlov’s dog instead of feeling free to roam the yard. A BPD mother may complain about enabling her children, but what she’s really doing is enabling herself to assume martyrdom via virtue signaling. Tendentious charity implies that the provider should be praised and the receiver should be grateful. Instead of promoting sustainable independence and healthy self-esteem, the provider maintains power through resource allocation while the receiver remains disabled. Overindulgence of any ilk, and the accompanying language of sacrifice and atonement, eventually becomes a bargaining device to discourage betrayal.
According to Tom Bunn, LCSW: “She cannot tolerate feelings of abandonment. She must, no matter what it does to the child, cripple at least one child so that the child will never, even as an adult, be able to leave her. This means destroying at least one child’s ability to function as an independent person. The child must never outgrown the feeling of being a part of the mother.” Or, as Dr. James Masterson put it, “There is a belief by each of them that if one dies, the other will die. The concept of emotional blackmail is now visible, for if a child believes their very existence depends upon their mother’s existence, and is thus responsible for her life, how can they venture far from her? What if she should have health problems and her child is not there to save her?” In summation, the self-sufficiency and potential self-actualization of the child is supplanted by time-released idealization and occasional donations to prolong a cycle of guilt and dependency that has been engineered by the mother to satisfy her own needs, albeit unconsciously. The Cluster B exchange rate inevitably leaves a trail of bemused children who feel ambivalent about their prospects for acquiring self-efficacy. In families where money and possessions are the currency of love, it’s like putting a fresh coat of paint on a house that’s already been eaten by termites.
Borderline mothers cannot tolerate separation, and their overbearing presence can feel suffocating, intrusive, or “cannibalistic” to her children as they attempt to claim sovereignty in adulthood. The children are instrumentalized as props to stabilize their mother’s unstable emotions while also serving as sympathetic subordinates to soothe her all-encompassing anxieties. A BPD mother clips the wings of her children because her own wings are not stable enough for flying solo in the stratosphere of life’s daily challenges. Reality, in its messiness and incompatibility with her cognitive distortions, dysregulates the Borderline mother, so she creates what amounts to her own reality and defends it with the tenaciousness of a bull shark. Whenever her children provide reassurance and emotional support, their efforts are randomly rewarded through a process of variant ratio scheduling (inconsistent praise via intermittent positive reinforcement) to keep her children compliant. Being defined by the gaze of the other, her most deferential children conveniently serve as endemic sources of regulatory supply. BPD mothers do not teach their children self-respect; they teach their children to respect the needs of their mother. Her rejection sensitivity and paranoia keep her in a constant state of agitation while seeking reassurance for her cognitive distortions caused by impaired reality testing. Likewise, the desperate neediness of the mother is usually reinforced by the approval-seeking behavior of her children. The child is searching for a “good enough” mother, but the mother is also a child searching for a “good enough” mother. After all, what child doesn’t yearn for love and approval from their parents? However, children who have surrendered themselves for the sake of parental acceptance (being defined by the Borderline) will invariably become more codependent over time—sacrificing their potential for fulfillment as adults. In addition, the mother’s need for control can undermine her children’s ability to express themselves, feel confident, establish boundaries with others, or take initiative. As a result, her children often feel emotionally paralyzed, defensive, guilty, and helpless while deferring to their mother’s relentless crusade for supremacy, similar to what happens during Stockholm syndrome.
In many ways, children of BPD mothers are not allowed to grow up because growing up represents a threat to the mother’s need for safety. In this sticky situation, the emotional dependency and psychological immaturity of the mother is projected onto her children to make them feel dependent on her. The mother’s fear of abandonment is often so insurmountable that the very idea of her children establishing a life of their own is considered a threat to her survival. Consequently, becoming mollification marionettes is easier for the children than trying to untangle the complicated web of psychological strings that resulted in submission and regressive enmeshment. Torn between a tale of two incompatible identities, her children are expected to regress into a realm of infantilism while taking on selective parenting roles. Regression keeps the mother from feeling threatened by her children’s natural progression towards adulthood, and parentification allows for comfort when the mother is seeking consolation, special assistance, guidance, or reassurance for her worldview and life choices. Ironically, the mother may later blame her children for their continued dependence while simultaneously disapproving of her children’s efforts to individuate—it’s like trying to escape a mobius strip. In other words, the psychological health and independence of her children triggers the mother’s worst fear: relinquishing emotional dependency. Incentivizing enmeshment is how the codependent sausage is made.
The mask of normality (false self) is perhaps the most impressive adaptive mechanism of people with Borderline Personality Disorder—a Trojan Horse for social acceptance and protective facade that facilitates interpersonal functioning. A Borderline mother’s false self could be thought of as a “surrogate self” that substitutes for what could have been or what should have been (i.e., integrated/ true self). The false self, transactional and superficial as it is, also belies how much people with this disorder struggle inside. Because the Borderline mother inhabits a dissociative self due to a lack of intrapsychic congruency, she must construct a functional cover through presentation management that allows her to mask her shadow self. Although her skin is thin, it’s highly polished and adept at deflection. Being “perfectly presentable” to an invalidating and abusive parent ensured acceptance during childhood, but it prevented the authenticity of identity that develops through healthy exploration and secure attachment. Subsequently, most Borderline mothers have perfected the art of being perfectly presentable between periods of dysphoria or anger and can switch to smiles on a dime when the threat of embarrassment shows up at their front door. As mentioned in The Borderline Koan, people with BPD can go “under the radar” for extended periods of time by appearing composed, charming, vivacious, affectionate, generous, glamorous, and ostensibly reasonable to those who encounter them during brief interactions (the halo effect). In due course, the Borderline mother becomes an imposter who succumbs to self-deception before deceiving others with her constructed persona. In addition to her varnished mannerisms, the BPD mother earnestly tries to maintain an internalized “good object,” which may include feelings of moral superiority, impassioned convictions, and redemptive vanity to offset her internalized “bad object,” which tells her that she is unattractive, inadequate, stupid, and worthless. BPD virtue signaling, for example, is an elaborate announcement to bolster the integrity of their good object, regardless of its proactive validity. This also explains the infamous mismatch between how people with this disorder want to bee seen versus how they really feel and behave when their insecurities are triggered. To make matters worse, the mother is saddled with feelings of guilt and shame that she attempts to discharge onto the nearest recipient, as if they were grounding conductors for her internal lightning storm.
While compensatory structures allow people with BPD to function well in most settings, defensive structures keep them in a perpetual state of anxiety that inevitably results in conflict. More importantly, dissembling prevents exposure, because exposure means death to the Borderline’s alloplastic defense mechanisms. Mirroring (emulating the behavior of others and/or appropriating their interests) also keeps the BPD mother from feeling estranged during social gatherings or interactions with intimate others. However, the Borderline’s public image is usually quite different from their private persona, especially when their precarious mood begins to shift during encounters with frustration. Stress, perceived rejection, and feelings of being disrespected typically precede defensive behavior designed to protect the mother’s fragile sense of self. If interpersonal conditions do not remain auspicious, the mother’s hostility will take the wheel (some people with BPD have a ceiling to their animus and episodic rage, while others do not). Even more disturbing, a subset of BPD mothers can deteriorate into a state of transient psychosis or secondary psychopathy under severe stress, hence commentary about Borderlines appearing “possessed” when splitting occurs. What an untreated Borderline is capable of when their back is against the wall is not suitable for all audiences, but this is also how they maintain control over their spectators.
Being masters of theatrical performance (psychodrama) and blame-shifting, Borderline mothers often convince acquaintances and concerned others that their primary difficulties in life are caused by ungrateful children, lackluster partners, evildoers, and “those damn people” (fundamental attribution errors). After all, mothers suffering from this disorder experience their interpretations as correct and subsequent reactions as self-justified, regardless of how far the lens of their inner world deviates from an accurate assessment of the outer world. No matter how misaligned such thoughts, feelings, and reactions might appear from an objective perspective, most Borderline mothers will find a way to pass customs without undergoing a search and seizure of their psychological baggage. When desperation is cornered, the ingenuity of the escape artist can be stunning. To control the narrative is how the war of public relations is won. Poor object relations and impaired reality testing combine forces with a high index of suspicion as the mother’s list of persecutors escalate beyond the event horizon. If she can’t trust the vicissitudes of her own mind, how can she trust anyone who lives outside of it? To be sure, an untreated Borderline mother needs to be counterbalanced by an exceptionally healthy partner for her children to prosper, but anyone who is truly levelheaded either wouldn’t stick around for long or remain healthy. Parental alienation, for example, happens when the mother triangulates the children against her spouse, resulting in even more discontinuity among family members. Co-parenting collapses and the children are forced to pick sides without understanding the real source of disharmony. As the art of projection reaches a fevered pitch, the mother conveniently avoids accountability for her unreasonableness and behavioral inconsistencies via plausible deniability, self-justification, blame, and intimidation. Developing insight is an inside job that externalizing disorders are not inherently equipped to handle.
As a reminder, untreated people with BPD do not see themselves as disordered (anosognosia) and believe passionately that their thoughts, feelings, and reactions are entirely justified. Being chronically irrational, Borderline mothers rely on emotional reasoning rather than logic and confuse their children during communication through selective memory (dissociative amnesia), dismissiveness, anger, or complete denial (there are significant neuroanatomical and functional differences in the BPD brain that also account for these unwelcoming responses). In other words, the mother’s memory is biased towards information that avoids personal blame and feelings of shame (emotional memory blocking). Revisionism is a Borderline trademark, despite the magnitude of historical evidence to the contrary. Sitting with uncomfortable feelings while mapping out the correct chronology of events is a job too great for those who prefer the safety of experiential avoidance. Whatever a person with BPD remembers during periods of conflict will always be someone else’s fault, because their hypersensitivity to mortification cannot tolerate the burden of developing insight or accepting accountability. BPD mothers do not have the temperament, maturity, or attention span to engage in emotionally challenging conversations, and they will preemptively shut down discussions that might lead to questioning their thoughts or actions. Even when a particular conversation seems normal or productive, the following is sure to plummet. No matter how tempting, her children should never broach topics that will trigger their mother’s reactivity. The children’s repeated attempts to JADE (justify, argue, defend, and explain), no matter how articulate or reasonable, never work. In reality, the better the child is at explaining themselves, the less they’re understood. The nuances of rationality and independent thought are a threat to the emotional biases of the mother because disagreement equals rejection. As a result, she will often tune out during serious discussions, which makes her children feel even more invalidated. To make matters worse, healthy communication is anathema because it triggers archaic fears associated with painful subject matter and threatens the adhesive strength of the trauma bond. Besides, even the most innocuous dialogue can be misinterpreted as confrontational commentary due to the Borderline mother’s keen sensitivity to tone of voice and her propensity for paranoia. In fact, some of the most protracted, profligate, and contentious conversations occur whenever children of the disordered try to extract order from their mother’s misconceptions, deflections, and bizarre digressions. Keeping things light and superficial is the only way to potentially avoid an avalanche of primitive defense mechanisms, and any discussion about the fact that mommy might be disordered typically backfires with a loud report (untreated people with BPD frequently feel offended rather than relieved by the suggestion that their symptoms stem from character disturbance, and this problem is undoubtedly made worse by the associated stigma surrounding Cluster B disorders). Unfortunately, the least effective people at convincing someone suffering from a personality disorder to seek specialized treatment are usually the individuals who are closest to them.
The Borderline mother’s lack of self-awareness is utterly astounding, but it’s a protective mechanism to avoid deep feelings of insecurity, self-loathing, guilt, and shame. Likewise, her abundant use of criticism and insults allows her to maintain a grandiose image to compensate for low self-worth via projection. Whatever is wrong, it can’t possibly have anything to do with her. In fact, the denial of the BPD mother can become so tenacious that her family lives in denial by proxy. In many ways, the mother’s full-time job is to convince herself and others that she is right about the nature of reality so that she can forever externalize whatever she is too afraid to acknowledge. However, never letting them see you sweat is the gateway to regret for families who embrace the alluring anesthetization of denialism.
“The mother may be blatantly ill, but more often her pathology is quite subtle. She may even be perceived by others as ‘the perfect mother’ because of her total ‘dedication’ to her children. Further observation, however, reveals her overinvolvement in her children’s lives, her encouragement of mutual dependencies, and her unwillingness to allow her children to mature and separate naturally,” states Jerold J. Kreisman, M.D.
Borderline mothers never learned to trust their environment while growing up because it was habitually unpredictable, invalidating, or filled with abject terror. Hypervigilant, suspicious, and mistrustful, the mother will often interpret innocuous comments, facial expressions, tone of voice, or humorous gestures as personal attacks, as evidenced by her paranoid inquiries, such as, “What did they mean by that?” or “What’s going on here?” Unsure of herself, she is unsure of others. There must be a hidden agenda; an ulterior motive; a sinister plan! After all, isn’t everyone competitive and untrustworthy? Moreover, the Borderline mother may have competed for her parent’s attention with other siblings, or she may have received validation within the family unit based solely on her performance. At other times, she may have only been noticed when she was in extreme physical pain, which explains why some Borderlines exhibit a penchant for malingering. In a home that’s gone haywire, there’s no such thing as self-acceptance, emotional equanimity, or self-love. You either succeed or you suffer until success is eventually conflated with suffering. Subsequently, the BPD mother’s relentless drive for perfectionism in childhood and adolescence resulted in trying to control anything that offered the promise of stability, safety, and validation in adulthood. This “passion for the perfect” is how high-functioning Borderline mothers are capable of accomplishing tasks that provide order, structure, and a solid formula for unambiguous results. Perfectionism is an amulet against feelings of unworthiness and shame, because the vulnerability of error is seen as an existential imperfection that must be hidden by preemptively finding flaws in others (people with BPD have a low bar when it comes to feeling humiliated). Likewise, combative self-absorption is seen as a strength because uncompromising endurance is the Borderline mother’s benchmark for prosperity. However strong she may believe herself to be, especially when she reviews her track record for resilience, real strength comes from facing painful emotions rather than compulsively seeking to control one’s environment. People with BPD are always on the lookout for injustice, but they’re too traumatized to consider how their unresolved trauma might be traumatizing others, which is why their loved ones inevitably “abandon” them. Unbeknownst to the mother, survival of the inconsiderate, no matter how formidable, includes an ironic lack of consideration for the very factors that perpetuate her suffering. The burden of her desperation sets her mind on fire as the flames colonize the psychic space of her children.
BPD mothers don’t improvise because they’re too obsessed with what can be finalized. Do not make any changes in their routine or you’ll see a mom get mean. Activities need to be formulaic to reduce uncontrollable variables that exacerbate fear and feelings of incompetence. Never underestimate the mother’s need for certainty and centrality. Everything must be done a certain way or there will be hell to pay. Inflexibility is a BPD hallmark, and paying attention to superficial details in a meticulous manner (hypervigilant myopia) is invariably more important than seeing the bigger picture. Task completion distracts the mother from uncomfortable feelings, such as boredom and emptiness. Although she seeks stability, she cannot tolerate the tranquility of long-term stability because it’s a foreign feeling to an impulsive mind waiting for the other shoe to drop. She must always keep herself busy; anything to avoid the void. While some Borderline mothers rely on drugs, alcohol, shopping, grooming, food, or sex for purposes of self-soothing, others seek absolute control of their surroundings to calm their nerves in a manner comorbid with Obsessive-Compulsive Personality Disorder. Likewise, situational inconveniences will not be tolerated. Ambiguity is the enemy and a vehement devotion to gaining the upper hand is the anodyne for feeling overwhelmed. This intensity of focus allows the mother to experience the gratification of being in command while providing a sense of order to temporarily assuage her tension. However, because solution implementation takes away from the mother’s need to identify with her problems, a continuation of chaos in some realm should be expected, thereby justifying her grievances and need for a sympathetic support system. The tedious assertions that no one can help her, no one understands, everyone is against her, and no one cares must be recycled at the Karpman Drama rendering plant. Ordinances set by the repetition-compulsion cycle charter are sacrosanct, because life is repeatedly viewed as a zero-sum contest and ruthless blood sport of a type that would make Thomas Hobbes seem like a motivational speaker. Ultimately, receiving attention for having problems is prioritized over the pursuit of viable solutions, and panic is punctuated at the expense of equilibrium. Catastrophizing is a close second cousin to its first cousin control on the branching tree of BPD symptomatology.
Borderline mothers do not recognize or respect the boundaries of their children. In fact, they don’t understand the definition of interpersonal boundaries because their household of origin was most likely a boundaryless hazard zone capable of shocking a wildlife biologist. Everyone is in everyone else’s business, and no one is immune to scrutiny, suspicion, or interrogation. Besides, boundaries are perceived as a form of rejection and indisputable evidence that others are up to no good. Furthermore, decimating boundaries opens the door to taking up more oxygen in the room with tales of persecution and demands for consolation. After issuing a fatwah against privacy, others are expected soak up the mother’s suffering through unmitigated availability, but even sponges have limits. Rational opposition is futile, and having a life outside of the mother’s sector of suffering is considered abandonment. Consequently, Borderline mothers will double down on their unreasonableness by resorting to bullying, intimidation, pouting, throwing tantrums, or weaponizing guilt if their children exercise the right to say “no.” BPD mothers often cause their children to feel self-conscious about making their own decisions; disagreeing; establishing limits, or trying to define territory within the family structure. It cannot be emphasized enough that separation is kryptonite for people suffering from BPD, and every word or action that suggests a whiff of dissent is taken personally. The desperation and fear of the mother intensifies whenever her children express opposition or demonstrate self-determination. In some cases, the children become rebellious and may engage in verbal or physical altercations in an attempt to assert their independence. The children may also find themselves in the habit of lying to their mother to avoid her wrath or making evasive excuses to escape the contagious anxiety of her distressed presence. Many children will say or do whatever is necessary to avoid conflict. However, when the mother shows insensitivity to her children’s misgivings, confabulation-imbued gaslighting and projection are the primary tools she’ll use for leverage against them. In other words, reality is revised and the children are either accused of wrongdoing or considered crazy and resistant for questioning the warped logic, anger, paranoia, need for control, and resistance of the mother. As the chips of experiential avoidance are cashed in, her children’s experiences, emotions, and insights are minimized, dismissed, or used against them in a preemptive power play. By trivializing her children’s concerns, often through the fallacy of relative privation, she prioritizes her need for centrality and the supremacy of her suffering. Unfortunately, “obedient” children inadvertently feed their mother’s pathology by acquiescing to her increasing demands and deferring to her warped version of events. Nonetheless, no matter what the children do to appease their mother, it’s never enough. This unsavory predicament is described in the following passage by the clinical psychologist Daniel S. Lobel: “Borderline mothers see their children as forever obligated to them by rite of birth. They feel entitled to demand from their children unlimited support and service. The dependency of the Borderline is so great that the child is always seen as coming up short with regard to meeting their needs. This often sets up the mother to be the victim and the child to be vilified.”
The story of a Borderline mother and her children is best explained as a union of misplaced sensitivity. The traumatized mother is hypersensitive to anything that makes her feel emotionally uncomfortable (people with BPD have a low emotional quotient, low distress tolerance, and exhibit high levels of arousal). Because the mother is always in survival mode, her stress is palpable and becomes an emotional contagion. In synchronized contrast, her children become hypersensitive to the emotional discomfort, labile moods, and anxieties of their mother. Not wanting to upset or disappoint her, the children begin to make conciliatory adjustments in their style of interaction (“walking on eggshells”) while diligently monitoring the moods of their mother (“reading the room”). When the mother insists that her children must care about her emotional needs and respect her most urgent concerns, the children become overly responsive to their mother’s illness and never develop healthy boundaries or the ability to properly take care of themselves. Overall, the children cannot relax or think clearly as they internalize their mother’s unresolved tension and sense of doom; orbiting around her centrifuge of breaking catastrophes. “Good” children make their mother feel comfortable and “bad” children make their mother feel uncomfortable, which places her children in a no-win situation when it comes to making independent decisions and achieving optimal emotional distance. The conditioned pattern of watching out for their mother’s hypersensitive reactions and responding with immediate attempts at remediation (codependence) subsequently bleeds into every problematic situation and stressful interpersonal dynamic that her children encounter for the rest of their lives, or until the spell is finally broken. Adult children of Borderline mothers often feel that their value is based on what they can do for others rather than for who they are, and this lamentable belief represents the core of codependent behavior. BPD is an impairment of the mind that demands unwavering accommodation at the expense of others. For her children to manage their own lives is perceived as an affront that provokes the Borderline mother’s separation insecurity and rejection sensitivity. To sabotage her children’s capacity for independence is how the Borderline mother circumvents loneliness, and her methods are protean. As night follows day, the children are eventually converted into anxiety-ridden radar detectors without a reliable rudder, just like their mother. Welcome to the emotionally entangled singularity project and its discontents.
Many years later, adult children of Borderline mothers may experience shock, incredulity, outrage, bewilderment, and resentment when they finally learn about the psychological anatomy and interpersonal repercussions of Borderline Personality Disorder. There’s also a compelling inclination among adult children of BPD mothers to relapse into previous patterns of pathogenic family interactions and denial after the game has finally been revealed. Being dragged back into the drama via masochistic surrender is just another example of how powerful FOG can be due to the gravity of codependency, normalization, and habituation. Rationalizing the irrational is to be expected, especially when the majority of a person’s life has been spent attending to the shifting needs of an emotionally unstable parent. In addition, children are evolutionarily programmed to defend their caregivers, even if it sometimes means throwing themselves under the bus. Making elaborate excuses for one’s mother is natural, and there’s a cultural maxim to respect your parents, but at some point there will be no excuse left for not seeing things as they really are. Nonetheless, we can respect people without respecting toxic behaviors, unhealthy patterns, and bad ideas. Denial subsidizes sickness, and postponing reality can have fatal consequences. Acceptance requires understanding, and understanding is the only way that forgiveness can have meaning. We must first understand our parents before we can understand ourselves, but understanding ourselves in relation to others can be a disheartening and disorienting endeavor, especially if we experienced a traumatic childhood, because it reminds us of our contentious origins and subsequent psychological disadvantages. A common statement made by adult children after educating themselves about this baffling disorder is: “I always knew that something was wrong with my mother, but I just couldn’t put my finger on it.” Connecting the dots becomes easier with physical distance, emotional distance, education, and time; but uncoupling from the hive mind by undergoing a separation-individuation process requires unwavering courage and unparalleled emotional strength (the project is akin to exiting a cult). To reveal a Borderline mother’s propensity for playing hide the ball requires her family to put down the Whac-A-Mole mallet used to extinguish her recurring plights. Unfortunately, those raised in chaotic family circumstances sometimes spend most of their adulthood trying to rework their childhood. Trauma bonds are exceptionally difficult to overcome, but it’s worth the emotional labor. Basically, children of disordered parents must learn how to prioritize their own needs after many years of being conditioned to put themselves last. However, a fear of failure and a fear of success often keeps children of Borderline mothers in motivational limbo. Disillusionment can be agonizing, but it’s necessary to disabuse yourself to avoid further abuse. Upton Sinclair once said, “It’s nearly impossible to get a man to understand something when his paycheck depends on him not understanding it.” To paraphrase Mr. Sinclair, it’s nearly impossible to get someone to understand the insidious influence of adverse childhood experiences when their survival depends on them not understanding it. Despite the onerous challenges of trauma recovery, wallowing in the wake of familial havoc is indisputably unhealthy and potentially lethal in the long run.
When the adult children of a Borderline mother finally come to terms with what happened during their formative years, a crushing sadness will prevail—sadness for the mother they never had; sadness for their mother’s condition; sadness for their own suffering, and a feeling of devastating loss for the years that were wasted. However, the stages of change that occur during any grieving process are necessary so that more favorable changes can eventually emerge. That being said, the bargaining stage of grief is perhaps the most difficult to overcome when emotionally detaching from a maternal trauma bond; but once the peak of bereavement abates, these epiphanies have a chance to become actualized. Deprogramming requires not only divorcing oneself from the trauma bond, but separating from the version of oneself that was vulnerable to such dynamics. The prohibition of self-discovery is a life-or-death mission for an untreated Borderline mother because she must protect the archaic airspace of her insatiable dependency needs, and this unspoken form of suppression is highly contagious. However, denial of the truth doesn’t make the truth disappear; it merely exposes a person’s inability to cope with it. As the saying goes, we’re only as sick as the secrets we keep. Or, as Henry Miller put it, “Once you have given up the ghost, everything follows with dead certainty, even in the midst of chaos.” Cognitive dissonance is resolved by maintaining psychological distance through separation after giving up all illusions of normal reconciliation and completing a familial vivisection. The only way for children to avoid feeling disabled by their mother’s need for control is to develop creative strategies in adulthood to disable the drama caused by recurring “mama trauma” (i.e., avoiding intense emotional engagement; learning to observe rather than absorb; building a support system outside of the family; studying the disorder and its effects on others; creating functional boundaries; psychological self-improvement, and seeking relational trauma therapy). In the fullness of time, unpacking this type of predicament can become a catalyst for self-discovery or a force multiplier for despair. On a more positive note, adult children may experience a deeper sense of compassion based on understanding their mother’s disorder in the light of her traumatic history rather than relying on superficial and transactional interactions under the guise of normalcy. As eloquently stated by Dr. Tara J. Palmatier, “Sacrificing yourself at the altar of someone else’s pathology is not a measure of your love for them, it’s a measure of your willingness to be abused by them.” Most importantly, children must accept the fact that their mother may never have the capacity to understand the negative impact she’s had or continues to have on her family.
No mother is perfect, but BPD mothers wish that they and their families were perfectible based on impossible standards that were usually set in motion by their own parents. Unfortunately, the problems that perfectionism creates (disillusionment, insecurity, shame, anxiety, paralysis by overanalysis, and relentless self-criticism) are far more damaging than the problems that perfectionism pretends to solve. Reverse engineering the psychological damage caused by interacting with a Borderline mother is an arduous and time-consuming process, but it should not be postponed for the sake of maintaining appearances. Believing that you don’t deserve to have a place at the table is a tragic death of prosperity that precedes biological death. If children are not allowed to trust their intuitions, they’ll never develop the capacity to believe in themselves. Likewise, potential is lost forever if we’re denied permission to reach our potential as separate individuals. Children need stability, confidence, consistency, and a strong sense of self-reliance to develop independence in adulthood; otherwise, they’ll blindly perpetuate the mindset of their mother without having the tenacity to flourish with generativity. Above all, they need to develop self-love by experiencing a second birth (psychological) from their mother that allows for freedom of thought and unencumbered expression of self.
As the Borderline mother ages, her intensity may diminish when she finally loses steam and relegates herself to a life of resentful dissatisfaction (the most extreme symptoms of BPD, such as impulsivity, often relinquish over time). With any luck, she may find another audience to take the place of her children. The reins of control will slowly unwind as the mother begrudgingly settles for disappointment in lieu of her strained efforts to sculpt the family according to her iron will. For other BPD mothers, their insatiable need for control will decidedly follow them to their graves, but hopefully before the family is forced to dig their own. Life is too short for marinating in a multigenerational melting pot of maladaptive misery.
As with all Borderline relationships, there are only three options for children to consider: Avoid, challenge, or appease. Most of the time, the children of BPD mothers find themselves reluctantly pedaling between all three positions or avoiding contact altogether. It’s not that BPD mothers don’t love their children, it’s that they don’t understand the meaning of mature love any more than they understand the meaning of what’s required for healthy relationships. Love is conflated with psychological and behavioral control to attenuate the mother’s fear of abandonment. Love is also conflated with abuse and emotional incest, as it was during her own childhood. The mother needs someone to love her, but love and concern are insufficient because she has not addressed the injuries of her past. Jealousy, neediness, control, shame, anger, and desperation are the antithesis of love; they’re manifestations of fear. The Borderline Mother was not loved, or not loved consistently by her parents, so she is lost and continually searching for what she does not understand. She only understands what she needs to feel better about herself in the face of ongoing suffering. Perhaps it’s most accurate to say that a BPD mother loves what her children represent (emotional security) and misattributes her need for external regulation as a justifiable maternal bond. She creates her own version of love and decrees by fiat that it’s the correct version. However, it’s a mutation of love born from the origins of a traumatic childhood. The mother must learn to face, accept, and resolve her core wounds, and her children must recover separately. Until that day arrives, BPD mothers will never understand or effectively love their children, because they were never permitted to understand or love themselves. In such families, regression is rewarded and autonomy is frowned upon or punished. The lifespan of this pathological dynamic causes children to become prevailing repositories for their mother’s projections if the gravity of this disorder is not comprehensively understood, dismantled, and repudiated.
It’s not fair what the Borderline mother went through during her childhood, but it’s also not fair what she’s capable of putting her family through because of it. Although neglect is a form of emotional abuse that most people suffering from this disorder unfortunately experienced, controlling others to avoid feeling neglected is also abusive. Nevertheless, Borderline mothers can be inspirational, affectionate, talented, intelligent, humorous, and situationally benevolent. When a Borderline mother is in a good mood, her magnetism is incomparable (this is also why it’s so difficult for family members to break free from the momentum of her dependency). A BPD mother often performs amazingly well at many things, except when it comes to relationships. She has the energy of a thousand suns, but anyone who gets too close will get burned until she accepts responsibility for the consequences of her disorder and commits to specialized treatment. BPD mothers are human beings, and informed observations about the effects of childhood trauma and mental illness are not meant to be merciless accusations. The task for adult children is to process this information with dispassionate honesty rather than capitulating to self-indulgent parent bashing. Animosity towards an affliction is not the same as animosity towards the afflicted. Borderline Personality is a disorder and not a choice; nonetheless, it’s expected that the family will be playing by the mother’s capricious rules and allowing her to take full control of the court. Borderline mothers are not casual cooperators because they insist on holding all of the cards that were unavailable to them in childhood. However, it must be understood that the Borderline mother needs her children more than they need her, but she has convinced them otherwise. Adult children must learn to trust their intuitions rather than acquiescing to the impulses, grievances, and demands of a disordered parent. If they don’t, they’ll eventually abandon themselves.
“Owing to a poorly defined sense of self, people with BPD rely on others for their feelings of worth and emotional caretaking. So fearful are they of feeling alone that they may act in desperate ways that quite frequently bring about the very abandonment and rejection they’re trying to avoid, and which therefore validates and reinforces their fears.” — (excerpt from Surviving a Borderline Parent: How to Heal Your Childhood Wounds and Build Trust, Boundaries, and Self-Esteem)
Borderline mothers are suffering from a complicated disorder that’s built upon a shattered bedrock of identity disturbance, cognitive distortions, developmental deficits, insecure attachment, emotional extremes, anxiety, fear, and a profound lack of insight. Without self-awareness, how could they possibly understand what’s required to optimize the well-being of their children? However, the legacy of trauma should not be perpetuated in the minds and lives of a mother’s children. There are some obligations that should never be fulfilled.
For more information:
Signs of a BPD Mother: How to Cope
https://www.regain.us/advice/parenting/11-signs-you-have-an-emotionally-abusive-mother/
https://www.reddit.com/r/raisedbyborderlines/new/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9806505/
https://www.psychologytoday.com/us/articles/200707/borderline-walking-the-line
https://www.bpdglobal.com/about/bpd-explained/
https://www.psychologytoday.com/us/blog/the-intelligent-divorce/201405/the-borderline-mother
https://psyche.media/growing-up-with-a-mom-with-bpd-1-the-four-types
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2819472/
Being Raised by a Mother With Borderline Personality Disorder
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3268672/
FAMILY GUIDELINES
Click to access 3685_BORDERLINEPDF.pdf
http://www.drettensohn.com/having-a-parent-with-borderline-personality-disorder-bpd/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6131660/
Click to access mahan-kors-simmons-macfie-2018.pdf
http://www.bpdcentral.com/blog/?Enmeshment-in-Family-Relationships-1-1-1-35
https://www.yourtango.com/2017307359/11-signs-you-were-raised-bad-parent-and-its-affecting-you-now
https://www.europsy-journal.com/article/S0924-9338(17)30456-X/fulltext
https://blogs.psychcentral.com/caregivers/2017/01/4-signs-you-have-a-mommie-dearest-parent/
https://www.psychologytoday.com/us/blog/the-intelligent-divorce/201503/is-your-mother-borderline
The impacts of being raised by a Borderline mother.
https://psychcentral.com/blog/emotional-incest-when-is-close-too-close/
https://patch.com/california/carlsbad/bp–how-mothers-spread-borderline-personality-disorde37ca7270a9
https://cooperativeparenting.com/being-raised-by-a-borderline-personality-disordered-parent/
https://www.mysideofthecouch.com/a-day-in-the-life-with-bpd.html
Borderline Personality Disorder
Resource and recovery site for family members of personality disordered individuals: https://outofthefog.website/
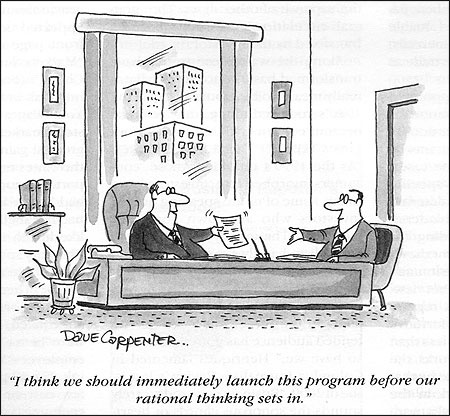
Knowledge can produce any change in the universe that’s compatible with its laws. — David Deutsch
Logic is a virtue only when it’s maintained as a method for reasoning. In addition, reasoning is a process rather than an abstraction. In other words, the rigorous application of logic is not exclusive to philosophical idealism.
Knowing how to think is invariably more important than knowing what to think. Processes matter. Likewise, in today’s onslaught of information overload, knowing what to get rid of can be as essential as knowing what to keep (e.g., a way of scrutinizing the landscape of our mind to eradicate what neuroscientist and psychologist Dean Buonomano described as “brain bugs”).
Formal logic consists of three basic rules of engagement that are operationally independent but mutually cohesive when analyzing propositions to develop a reliable framework of epistemology.
1. Inductive reasoning: Specific premise to a general conclusion.
2. Deductive reasoning: General premise to a specific conclusion.
3. Abductive reasoning: Most likely explanation given all available data.
However, regarding the seemingly infinite abyss of logical fallacies and their increasing regularity in daily conversation, there are five particular travesties of cognition that I encounter as a clinician more than I care to document during any given session. In addition, given today’s inauspicious trend of factual relativity and a blatant disregard for expertise, the need for intellectual vigilance has become something of a moral emergency among those still concerned with the concept of truth.
1. The fallacy of illicit transference is an informal fallacy that is committed when an argument assumes there is no difference between a term in the distributive (referring to every member of a class) and collective (referring to the class itself as a whole) sense. This fallacy occurs within two categorical errors: What is true of the part is true of the whole (composition), or what is true of the whole is true of the part (division).
Examples: {A} This politician in corrupt; therefore all politicians are corrupt (composition). {B} This agency is known for malfeasance; therefore any employee of this agency is untrustworthy (division). * Anomaly hunting is a common, supplemental approach to this fallacy in which an individual searches for confirmation of a belief while ignoring information that refutes their belief.
2. Post hoc, ergo propter hoc is a logical fallacy that infers the premise that if something occurs after an event, it must be caused by the event; used to indicate that a causal relationship has erroneously been assumed from a merely sequential one.
Example: The WTC 7 building in New York City (north of the Twin Towers) was known to contain private, financial banking records and collapsed shortly after the initial 9/11 attacks; therefore an attempted cover-up of fraudulent banking practices explains why 9/11 was an inside job orchestrated by the government via controlled demolition. Obviously, correlation does not prove causation. However, efforts to preoccupy oneself with erroneous associations often persist long after additional evidence has been produced to falsify such claims (e.g., the Backfire Effect).
3. Just-World Hypothesis (aka the Just-World Fallacy) is the assumption that a person’s actions are inherently inclined to bring morally fair and fitting consequences to that person, to the end of all noble actions being eventually rewarded and all evil actions eventually punished.
Example: People get what they deserve. This idea also derives from the presupposition that the world is an “equal playing field,” or that a person has unmitigated free will to “choose otherwise” (also known as a fundamental attribution error).
4. Argumentum ad populum is a logical fallacy that occurs when something is considered to be true or good solely because it is popular.
Example: Millions of people agree with my viewpoint; therefore, it must be right.
5. The Nirvana Fallacy is the informal fallacy of comparing actual things with unrealistic, idealized alternatives. It can also refer to the tendency to assume that there is a perfect solution to a particular problem (e.g., the perfect solution fallacy).
Examples: {A} Seat belts are a bad idea because people are still going to die in car crashes; therefore wearing a seat belt is an unecessary precaution. {B} Either there is a perfect solution to ending gun violence, or we shouldn’t do anything about it at all.
Alleviating the tyranny of confirmation bias prevents us from assuming the answers before investigating the questions. The facile satisfaction of asserting a comfortable narrative to explain complex or uncomfortable circumstances may be alluring, but it’s not a reliable way to understand the world and can result in the collateral damage of equal-opportunity credulity. In contrast, the psychological dividends available from exercising critical thinking skills allow us to remain honest while providing the most effective strategies for comprehending, accepting, and adapting to the nature of reality.